Conditions We Treat for Women
General
Pelvic Pain
Pelvic pain is women is a common symptom, which accounts for up to 30% of visits to a gynecologist, yet it is thought that close to 70% of cases of pelvic pain are not of a gynecological origin. By definition chronic pelvic pain is defined as pain which it is present for 6 months or longer, is localized to pelvis and is severe enough to cause functional disability requiring treatment. It is estimated that chronic pelvic pain affects 15% of women in United States sometime during their lifetime, yet almost 60% of those patients do not have a proper diagnosis (and therefore treatment). This is due to the fact that this pain usually spans more than one specialty, and treatment requires physicians who are specifically trained in chronic pelvic pain. Those statistics are even more staggering because over 20% of women with pelvic pain miss work, close 50% feel depressed and in 90% of women it affects their sexual life. Pain during or complete inability to have intercourse significantly affects personal relations between the patient and her partner and further adds to suffering. Despite the fact that chronic pelvic pain in women is more common than coronary artery disease, asthma or migraine headaches very few physicians specialize in its treatment. Pain is often blamed on psychological issues and patients are often referred to a mental health provider, instead of getting treatment for their true, existing disease.
Multiple conditions may cause pelvic pain and often they coexist together in one patient. Some of the more common conditions are:
- Endometriosis
- Interstitial cystitis/bladder pain syndrome
- Irritable bowel syndrome
- Spastic pelvic floor syndrome
- Adhesions in the pelvis and abdomen
- Pelvic congestion syndrome
- Pelvic nerve neuralgias
- Pain caused by pelvic mesh
Arizona Center for Chronic Pelvic Pain offers comprehensive treatment for those and many other conditions causing pelvic pain.
Overview of Pudendal Neuralgia
Pudendal neuralgia is a condition that affects the pudendal nerve, which transmits sensory information from the perineal region to the brain. People who experience pudendal neuralgia often describe it as a burning, shooting, or stabbing pain in the pelvic region.
-
Diagnosis of Pudendal Neuralgia
To diagnose pudendal neuralgia, healthcare professionals may utilize nerve conduction studies. These studies evaluate the electrical signals transmitted along the pudendal nerve, helping to identify any abnormalities or impairments. This diagnostic tool can provide valuable insights into the functioning of the pudendal nerve and assist in formulating a treatment plan.
-
Causes of Pudendal Neuralgia
One of the primary causes of pudendal neuralgia is pudendal nerve entrapment syndrome. This occurs when the pudendal nerve becomes compressed or trapped, leading to pain and discomfort in the pelvic area. Advanced practitioners, such as physical therapists specializing in pelvic health, can work alongside healthcare professionals to address this condition comprehensively.
-
Treatment Options for Pudendal Neuralgia
Various treatment options are available for managing pudendal nerve pain. Pudendal neuromodulation, for instance, has shown promise in providing relief to individuals experiencing pudendal neuralgia. This technique involves implanted devices delivering electrical impulses to the pudendal nerve, helping to modify and alleviate pain signals.
-
Impact on Sexual Health
Pudendal neuropathy, another term often used to describe pudendal neuralgia, can have a significant impact on sexual health and function. Many individuals with this condition may experience sexual dysfunction, such as pain during intercourse or diminished sensation in the genital area.
Addressing sexual health concerns should be approached holistically, with input from healthcare professionals specializing in both pain management and sexual health.
-
Perineal Pain and Its Management
Perineal pain is a common symptom associated with pudendal neuralgia, and it can be highly debilitating. This type of pain is often described as occurring in the area between the anus and genitals. Understanding the neuropathic nature of this pain is crucial, as it helps guide treatment strategies and ensures that appropriate interventions are employed to alleviate discomfort effectively.
-
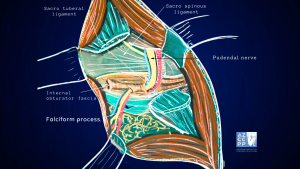
Understanding Entrapment Syndrome
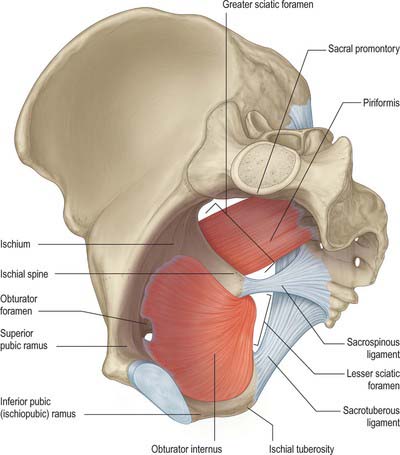
Addressing pudendal neuralgia requires a comprehensive understanding of entrapment syndrome, as it plays a significant role in the development and progression of the condition. For example, the sacrospinous ligament has been named as a place where nerves can get pinched, leading to damage to the pudendal nerves and pain.
This knowledge allows for more targeted approaches to treatment and potential surgical decompression options for those who do not respond adequately to conservative management.
-
Educating Individuals About Pudendal Neuralgia
By educating individuals about pudendal neuralgia and its symptoms, we contribute to a greater understanding of this condition. Health encyclopedias and informational resources are invaluable tools in disseminating accurate and helpful information to those seeking knowledge about their condition. Empowering individuals with knowledge enables them to make informed decisions regarding their healthcare and seek appropriate treatment and support.
- Comprehensive
Care and Management
Pudendal neuralgia is a complex condition that can significantly impact pelvic health and sexual function. With the guidance of healthcare professionals and advanced practitioners and the use of diagnostic tools like nerve conduction studies, we can better understand and effectively manage pudendal nerve pain.
By exploring treatment options such as pudendal neuromodulation and addressing related symptoms like sexual dysfunction, we can strive towards improving the quality of life for individuals with pudendal neuralgia.
Pudendal Neuralgia: Relatively Unknown Cause of Severe Pelvic Pain
In my practice, I define it as pain located in the area of innervation of the pudendal nerve. Pudendal nerve entrapment is an impingement of the pudendal nerve due to scar tissue, surgical supplies, or mesh. Pudendal nerve entrapment is, therefore, one of the causes of pudendal neuralgia.
However, other causes, such as inflammation, spasms of the surrounding muscles, or other nerve diseases, may also be a reason for pain.
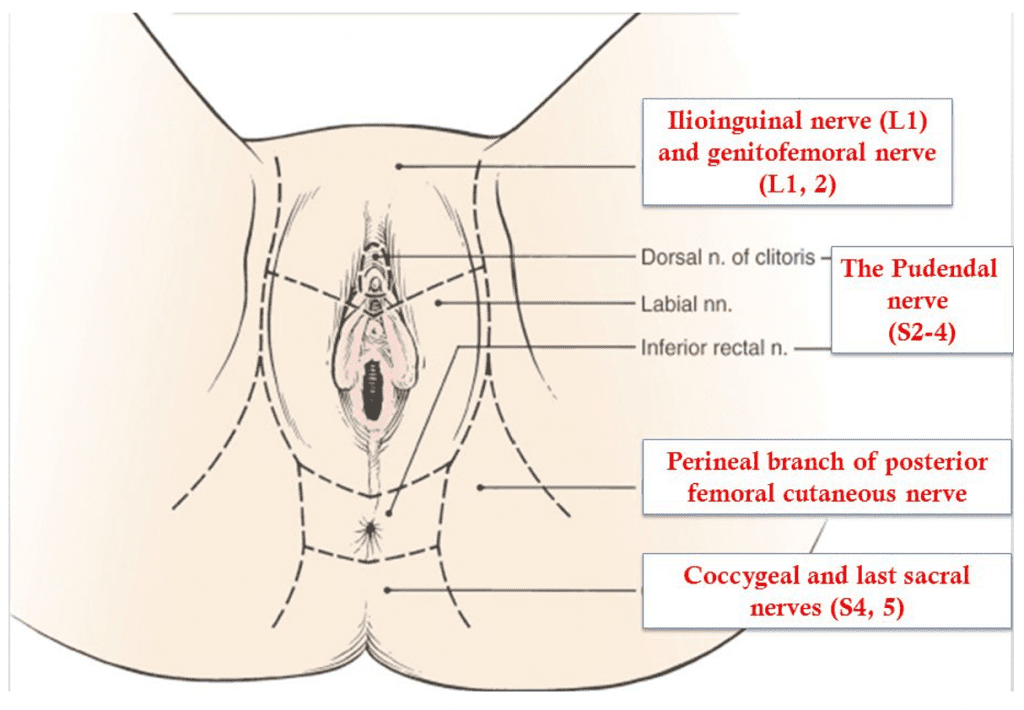
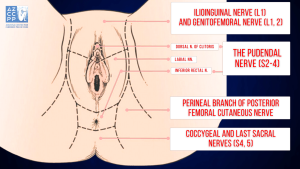 Innervation of the Perineum
Innervation of the Perineum
Pudendal nerve entrapment is almost always caused by a traumatic event in the pelvis. This may include pelvic surgery (with or without mesh), difficult childbirth, athletic injuries, falls, and other accidents. A repetitive injury, such as bicycle seat pressure on the pelvic floor, may also lead to pudendal nerve entrapment (cyclist syndrome).
Diagnosis of pudendal nerve entrapment is not easy and relies heavily on taking a detailed history. Pain is located in the vagina, vulva, clitoris, perineum, and rectum, and it may involve one or all of those areas. Pain is more severe when sitting than when standing or lying down, and sitting on the toilet is generally better than sitting on a chair.
Most of the patients with real nerve pain injuries have pain on one side only, or one side is significantly more painful than the other. Chronic Pelvic Pain is generally more severe with urination, bowel movements, and intercourse. Some patients may also have difficulty emptying their bladder (hesitancy) and bowel (constipation).
One of the most debilitating symptoms of pudendal nerve entrapment is a sensation of continuous sexual arousal (persistent genital arousal disorder, or PGAD). Patients often reduce this sensation through masturbation, which only provides temporary relief.
Nantes Criteria
My mentor, Professor Roger Robert, a pioneer in the treatment of pudendal nerve entrapment, has developed Nantes criteria that greatly assist in diagnosing this condition. Studies have shown that patients who more closely meet the criteria have better outcomes from the surgical decompression of the nerve.
Inclusion Criteria |
|
Exclusion Criteria |
|
Complementary Criteria |
|
Associated Signs |
|
Inferior Rectal Nerve |
Cutaneous Branch of the Obturator Nerve |
Lateral Cutaneous Branch of Iliohypogastric Nerve |
Femoral Branch of Genitofemoral Nerve |
Posterior Femoral Cutaneous Nerve |
Lateral Femoral Cutaneous Nerve |
Iliohypogastric Nerve |
Clitoral/Perineal Nerves |
Femoral Nerve |
Genital Branch of Genitofemoral Nerve |
Other Nerves Innervating the Pelvis |
Pain in pudendal nerve entrapment is of a neuropathic nature, which means that patients feel burning, tingling, and numbing sensations (paresthesia). Some patients have the sensation of a foreign body located in the rectum or vagina (allotriesthesia) and may describe it as a “red hot poker” in the rectum.
Some patients do not experience any chronic pain but have complete or partial numbness in the area of innervation of the pudendal nerve.
Extra tests, such as magnetic resonance neurography (MRN), pudendal nerve motor terminal latency (PNMTL), another electrophysiologic test, or sensory threshold testing, can usually not determine if someone has pudendal nerve entrapment.
An important part of the Nantes criteria is a CT-guided pudendal nerve block, which is used to find and treat pudendal nerve entrapment. If pain doesn’t go away right away after a CT-guided pudendal nerve block, it’s likely that the pudendal nerve is not the source of the pain.
Conservative Treatments of Pudendal Neuralgia
Pudendal neuralgia is a challenging condition that can cause significant discomfort and impact daily life. Fortunately, there are various conservative treatments available to help manage the symptoms and improve quality of life. This guide provides an overview of effective non-invasive methods that can be employed to alleviate pain and protect the pudendal nerve.
-
Avoidance of Additional Injury
Patients must immediately cease activities that lead to nerve injury. For example, if pudendal neuralgia was caused by riding a bicycle, the patient should stop cycling immediately. Avoiding such activities is crucial to prevent further damage to the nerve. However, this approach may not be feasible in cases where the patient develops pudendal neuralgia as a result of surgery or childbirth.
-
Nerve Protection
Protecting the pudendal nerve is vital for managing pain and preventing further injury. This can be achieved by using specialized sitting cushions that relieve pressure on the pelvic area, zero-gravity chairs that distribute weight evenly, or kneeling chairs that reduce strain on the lower back and pelvis. These tools help minimize discomfort and protect the nerve from additional stress.
-
Medications
Various medications can be used to manage the pain associated with pudendal neuralgia. Oral medications, such as anti-inflammatory drugs, muscle relaxants, and pain relievers, can provide relief. Additionally, vaginal or rectal suppositories can deliver medication directly to the affected area, offering targeted pain relief and reducing inflammation.
-
Pelvic Floor Therapy
Appropriate pelvic floor physical therapy can play a significant role in managing pudendal neuralgia. This therapy aims to minimize pelvic floor muscle spasms, which can contribute to nerve pain. Physical therapists specializing in pelvic health can develop personalized exercise and stretching routines to improve muscle function and reduce tension in the pelvic region.
-
Botulinum Toxin A Injections
Botulinum toxin Injections, commonly known as Botox, can be administered to the pelvic floor muscles to alleviate muscle spasms. By relaxing the muscles, these injections can reduce pressure on the pudendal nerve and provide relief from pain. This treatment option is often used in conjunction with other conservative therapies for maximum effectiveness.
-
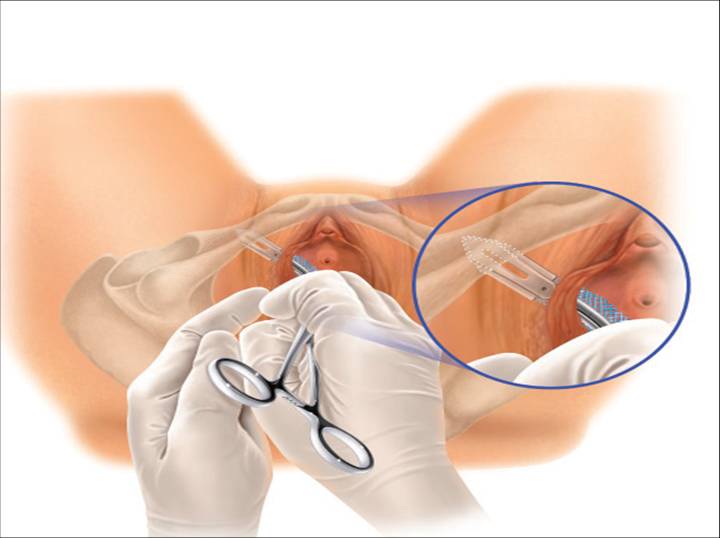
Pudendal Nerve Blocks
Pudendal nerve blocks involve the injection of an anesthetic and/or steroid medication near the pudendal nerve to reduce pain and inflammation. These injections can be guided by CT or ultrasound imaging, or they can be performed unguided transvaginally. The goal is to restrict the nerve as it enters the lesser sciatic foramen, 1 cm inferior and medial to the sacrospinous ligament-ischial spine attachment. This procedure can provide temporary relief from pain and is often used as a diagnostic tool to confirm the source of pain.
-
Pudendal Nerve Injections
Injections containing amniotic fluid and a liquified amniotic membrane can be used to treat pudendal neuralgia. These injections provide anti-inflammatory and regenerative properties, promoting healing of the nerve. The use of amniotic products can help reduce pain and improve nerve function over time.
-
Ablation Procedures
Pulsed radiofrequency ablation (pRFA) and cryoablation are minimally invasive procedures that can be used to treat pudendal neuralgia. pRFA uses electrical pulses to disrupt pain signals and reduce nerve sensitivity, while cryoablation involves freezing the nerve to block pain transmission. Both techniques aim to provide long-lasting pain relief and improve the patient’s quality of life.
-
Nerve Stimulators and Spinal Cord Stimulators
Implantable devices, such as nerve stimulators and spinal cord stimulators, can be used to manage chronic pain in pudendal neuralgia. These devices deliver electrical impulses to the pudendal nerve or spinal cord, disrupting pain signals and providing relief. They are typically considered when other conservative treatments have not been effective.
-
Surgical Decompression of the Nerve
Surgical decompression of the pudendal nerve can be performed using several different approaches, including transgluteal, transischorectal, transperineal, and laparoscopic/robotic techniques. The goal of the surgery is to free the nerve from any entrapment or compression, thereby reducing pain and improving function. This option is usually considered when conservative treatments have failed to provide adequate relief.
Professor Roger Robert first described the transgluteal approach in Nantes, France, after which I significantly modified it. This approach offers, by far, the best access to the pudendal nerve, therefore allowing for the most complete decompression.
One of the technique’s earlier drawbacks was cutting the sacrotuberous ligament, which, in some cases, could lead to pelvic instability. However, the risk of that instability was eliminated when I began repairing the sacrotuberous ligament.
Cutting that ligament frees the nerve from scar tissue or surgical materials and allows access to the nerve. However, the sacrotuberous ligament should be fixed after nerve decompression is complete.
Other Modifications I Have Introduced to the Pudendal Neurolysis Surgery
In order to enhance the outcomes of pudendal neurolysis surgery, I have introduced several modifications to the procedure. These modifications are designed to improve visualization, ensure nerve integrity, manage pain more effectively, and promote better healing. Below are the key changes I have implemented:
-
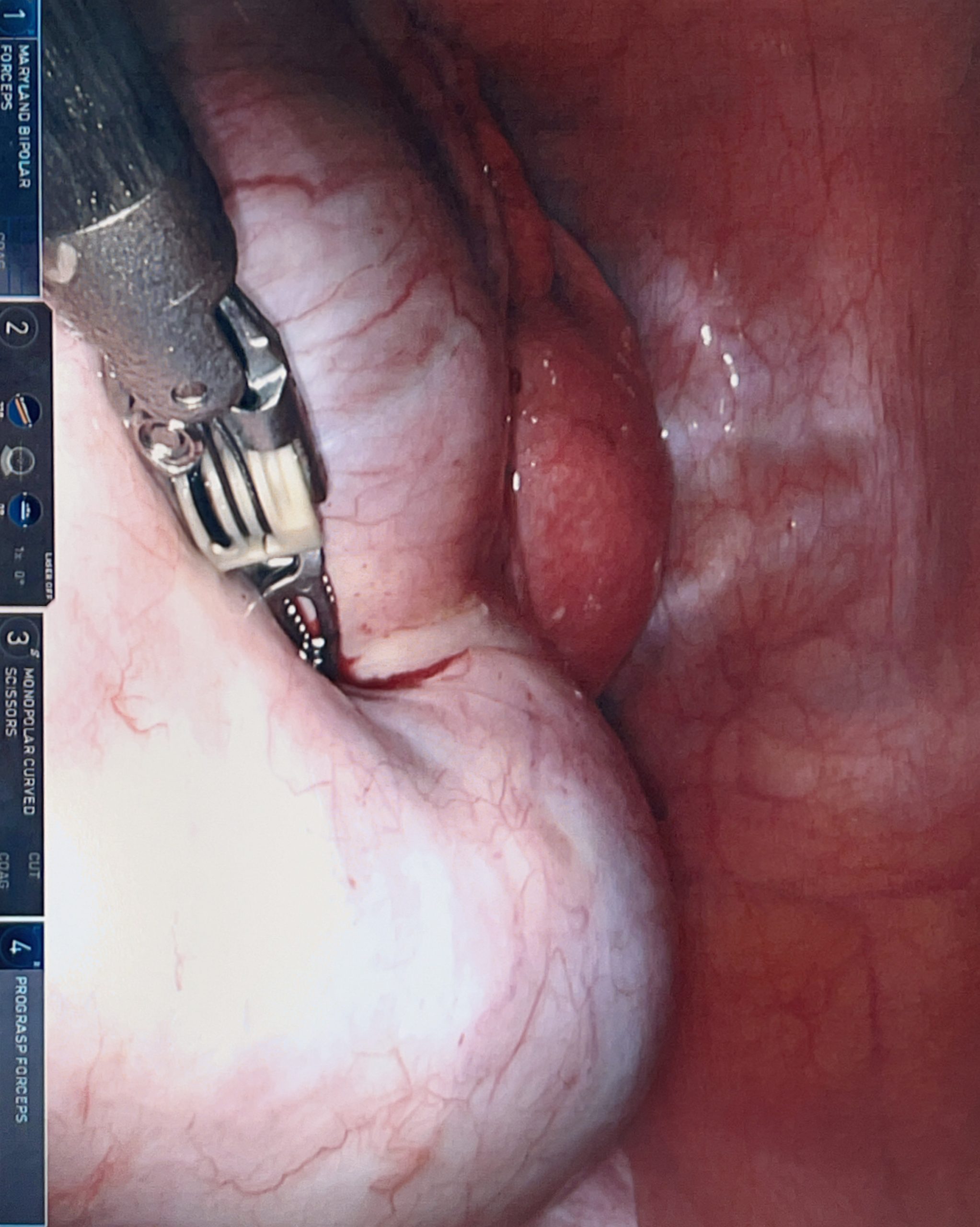
Use of Surgical Microscope
The use of a surgical microscope allows for better visualization of the nerve and the surrounding structures. This enhanced visualization is crucial for precise dissection and identification of the pudendal nerve, reducing the risk of accidental damage to the nerve and improving surgical outcomes.
-
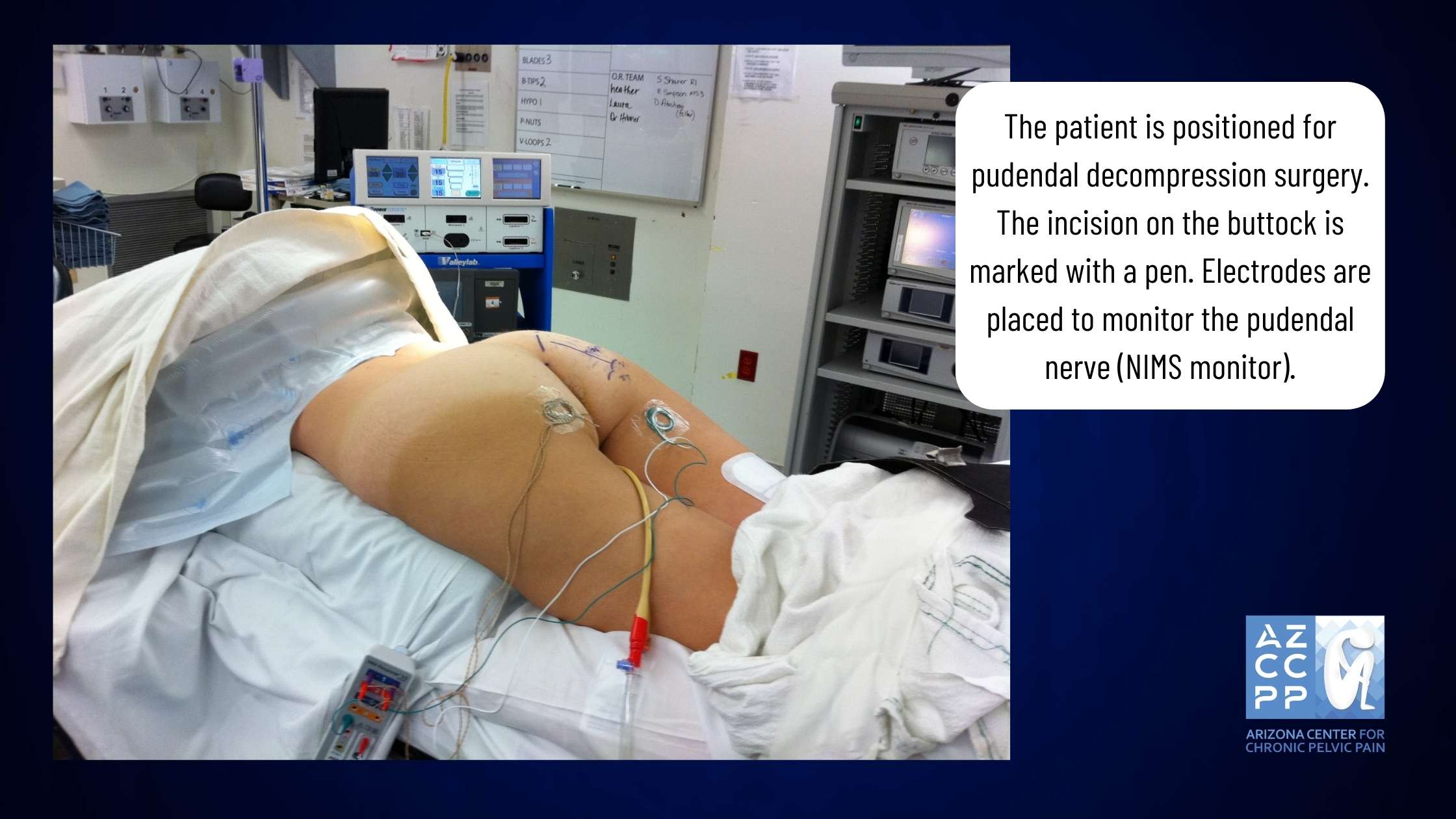
Nerve Integrity Monitoring System (NIMS Monitor)
The Nerve Integrity Monitoring System (NIMS monitor) can help identify the pudendal nerve. This system is especially helpful in cases where the nerve is significantly scarred or in repeat surgeries where the anatomy may be altered. By providing real-time feedback on the nerve’s function, the NIMS monitor helps ensure that the nerve is properly identified and preserved during the procedure.
-
Pain Pump
The use of a pain pump that delivers a local anesthetic to the nerve for about seven days after surgery can significantly decrease pain levels. This continuous infusion of anesthetic helps to reverse central sensitization, which is the memory of pain in the brain. By reducing pain and central sensitization, patients may experience a faster recovery and resolution of pain after surgery.
-
Nerve Wrapping with Adhesion Prevention Barrier
Nerve wrapping with an adhesion prevention barrier decreases the risk of scarring or re-scarring of the nerve after surgery. Several years ago, I switched from regular nerve wraps to wrapping the nerve with an amniotic membrane product.
In addition to anti-adhesion (anti-scarring) properties, the amniotic membrane contains nerve growth factors that promote nerve healing. It also may have the ability to attract your own body’s stem cells close to the nerve, which further helps with nerve regeneration.
-
Use of Suction Dressings
Using suction dressings after closing the skin helps minimize the risk of wound infection. These dressings create a vacuum effect that promotes better healing by reducing the accumulation of fluids and decreasing the chances of bacterial growth in the surgical site.
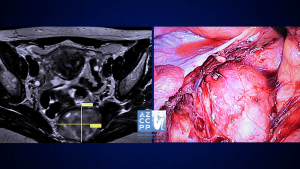 A microscope is used for transgluteal pudendal surgery, with a NIMS monitor for monitoring the nerve during surgery.
A microscope is used for transgluteal pudendal surgery, with a NIMS monitor for monitoring the nerve during surgery.
Laparoscopic/robotic procedures are less invasive, but they do not offer as good access to Alcock’s canal as transgluteal procedures do. It may be effective in cases where the nerve compression is limited to a small area, but the location of the compression may be difficult to determine prior to surgery.
In my practice, I perform both transgluteal and robotic nerve decompression procedures, but I believe that since the transgluteal technique offers better access and allows for decompression of the larger part of the pudendal nerve, it should be a preferred approach.
Even though the recovery time is longer compared to the laparoscopic procedure, the benefits of more complete nerve decompression are very important when considering the choice of surgery.
Overall, the surgery results show that most patients have significantly decreased pain and benefit from pudendal nerve decompression procedures.
If you or someone you know experiences pain from sitting in the clitoris, vulva, penis, scrotum, perineum, or rectum, call 480-599-9682 or email [email protected] to learn more about available treatments.
 View of the pudendal nerve through the microscope (nerve in the blue rubber band—vessel loop)
View of the pudendal nerve through the microscope (nerve in the blue rubber band—vessel loop)
What to Expect Before and After Transgluteal Nerve Decompression Surgery
Transgluteal nerve decompression surgery can be a crucial step in managing the debilitating pain caused by Pudendal Neuralgia. Understanding what to expect before and after surgery is essential for a smooth and successful recovery process. Here’s a comprehensive guide to help you navigate the journey:
-
Pre-Surgery Non-Invasive Methods
Before surgery, Dr. Hibner and his team will use noninvasive methods, such as physical therapy, suppositories, oral medications, nerve ablations, and amniotic fluid or membrane product injections, to help manage your pain.
-
Collaborative Decision for Surgery
The decision to undergo surgery is made collaboratively between you and Dr. Hibner, considering your medical history, exam results, radiology findings, and any additional testing. Surgery is considered when all conservative treatments have failed.
-
Surgical Approach and Pre-Operative Instructions
Dr. Hibner’s preferred method is transgluteal pudendal nerve decompression to free the nerve from scar tissue. In some cases, a robotic or alternative approach may be chosen. Follow all pre-operative instructions provided during your visit.
-
Surgery Positioning and Incision
During the surgery, you will be positioned prone (on your abdomen), and an incision will be made on the operated side of your buttock, measuring 2 to 4 inches.
-
Recovery Room Experience
After surgery, you will wake up in the recovery area with a bladder catheter, a pain pump delivering local anesthetic to your nerve, and a negative pressure dressing on the incision. You will receive a bag for the pain pump and a suction device for the dressing.
-
Post-Surgery Pain Management
You should feel numbness in the pudendal nerve area (where the pain was before surgery), but the buttock incision will be tender. The pain pump medication targets nerve pain and does not reach the muscles or skin of the buttock.
-
Hospital Stay and Activity Recommendations
Most patients spend one night in the hospital, with rare cases requiring a two-night stay. Be active and try to walk with support the day after surgery to prevent muscle loss and reduce the risk of nerve scarring. Avoid pulling the pain pump while moving.
-
Discharge and Home Care Instructions
You will be discharged with pain medications, instructions on using the pain pump, and a negative pressure dressing. You may need to return to the clinic for dressing and pain pump removal, or you may be instructed on how to do it yourself. Pain may increase temporarily after the pain pump is removed.
-
Showering and Travel Guidelines
You can shower two days after surgery but should avoid getting the incision area wet. Use a large garbage bag to protect the area during showers. Most patients can travel within 5-7 days after surgery, but a longer stay is recommended before returning home.
-
Activity and Physical Therapy
Resume activities gradually, avoiding actions that significantly increase pain. Avoid sitting, and if surgery was done on one side, sit only on the opposite buttock. Do not flex your hip(s) over 90 degrees to protect the repaired sacrotuberous ligament, which takes about six months to heal. Pelvic floor physical therapy should resume approximately six weeks after surgery.
-
Pain Improvement and Follow-Up
It may take 3–4 months to start feeling pain improvement. Continue taking all medications until advised otherwise, and reduce narcotic pain medications as instructed. Maximum healing may take 18 to 24 months, with most patients experiencing less or no pain after two years. If pain persists, additional solutions will be explored.
Outcomes
The outcomes of this procedure depend on the causes of nerve compression, the degree to which the nerve was compressed, and how much time elapsed between the injury and surgery. Unfortunately, the degree of nerve damage is difficult to assess before surgery.
From my extensive experience of doing hundreds of pudendal decompression surgeries, approximately two-thirds (66%) of patients benefit from this procedure. This number includes all the patients, even those with severe nerve injuries. That means that patients with less severe nerve injuries may benefit from the procedure even more.
A Little History
The book “The Change of Life in Health and Disease,” published in Philadelphia in 1871, established pudendal neuralgia as a medical condition. Knowledge of pudendal neuralgia was almost lost until the late 1980s.
French neurologist Dr. Gerard Amarenco reported on a series of patients with “syndrome du cyclist,” the cyclist syndrome, which occurs when a pudendal nerve is compressed between a narrow bicycle seat and the medial surface of ischial tuberosity (sitz bone).
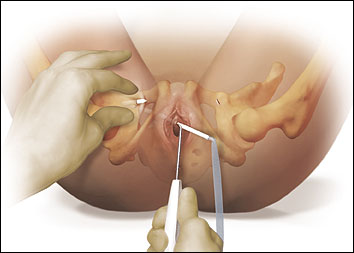
Dr. Ahmed Shafik, an Egyptian surgeon, first described how to surgically decompress the pudendal nerve using the transperineal technique (an incision around the anus) in 1992. Soon after, my mentor, Professor Roger Robert from Nantes, France, described transgluteal pudendal neurolysis—decompression of the pudendal nerve with an approach through the buttock.
Professor Robert is not only an outstanding neurosurgeon but also an anatomist, and this unique combination allowed him to develop a whole new procedure for pudendal nerve decompression.
I graduated from my fellowship in gynecologic surgery at the Mayo Clinic in 2003 and opened a pelvic pain practice in Phoenix in 2004. I started seeing patients with pelvic pain whose condition I was unable to explain using any known diseases.
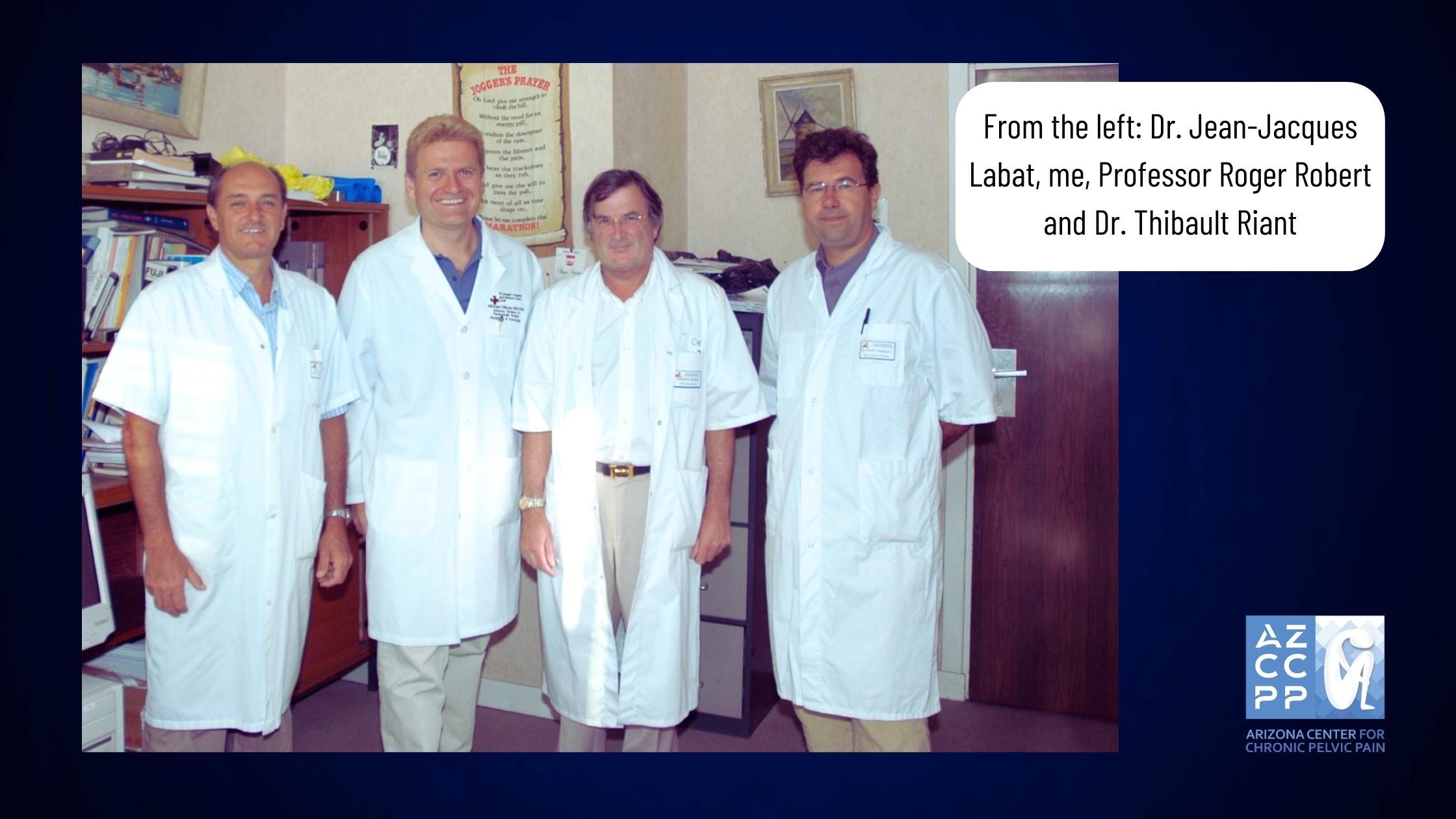
So, in early 2005, I googled the symptoms: perineal/vaginal burning pain with sitting. Several medical articles showed up, but most of them had one common name as one of the authors: Roger Robert. I then wrote to Professor Robert in Nantes, France, asking if I could come and learn from him.
In the summer of 2005, I traveled to Nantes and worked with Professor Robert for almost 3 weeks, assisting him with numerous surgeries and seeing many patients in the office with him.
I also worked with the wonderful Dr. Jean Jacques Labat, a neurologist who assisted Professor Robert with diagnosing and treating patients before surgery, and with the amazing radiologist Dr. Thibault Riant, who taught me how to perform CT-guided pudendal nerve blocks.
When I returned to Phoenix, I started seeing more and more patients with pudendal neuralgia and pudendal nerve compression, and I performed my first transgluteal pudendal nerve decompression in the fall of 2005.
The patient developed pudendal neuralgia after the removal of Bartholin’s gland. She did well after surgery, and soon, many more patients followed. I started modifying the original method that my great mentor, Professor Robert, had created from the very first surgery. The first modification was the repair of the transected sacrotuberous ligament.
There was a concern that leaving this ligament unrepaired may cause instability in the sacroiliac joint. So, from the very first patient, I would repair the sacrotuberous ligament the same way that an orthopedic surgeon repairs a ligament in the knee.
Next, I incorporated the use of a neurosurgical microscope into the procedure. This allowed for significantly improved precision.
The next modification was the use of an On-Q pain pump placed next to the nerve towards the end of surgery to provide postoperative analgesia and decrease central sensitization (memory of pain in the brain). In the third change, NIMS (nerve integrity monitoring system) was added so that the nerve could be found even when there was a lot of scarring.
The next modification was the use of nerve wrap to prevent the reoccurrence of adhesions. Initially, I was using a collagen nerve conduit, but a few years ago I switched to an amniotic membrane, which, in addition to preventing adhesions, also contains factors/chemicals promoting nerve healing.
The last major modification was the method by which I cut the sacrotuberous ligament. Cutting it in a Z fashion allows me better access to the nerve and facilitates the repair at the end of surgery.
Up to today, I have done several hundred of those procedures, most likely more than any other provider, with the exception of my amazing mentor, Professor Roger Robert.
For More Information, Visit:
https://www.glowm.com/section_view/heading/pudendal-neuralgia/item/691
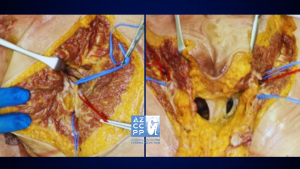
 Drawing of the steps of transgluteal pudendal neurolysis by Professor Roger Robert
Drawing of the steps of transgluteal pudendal neurolysis by Professor Roger Robert
 View of the opened space between the sacrotuberous and sacrospinous ligaments by Roger Robert
View of the opened space between the sacrotuberous and sacrospinous ligaments by Roger Robert
One of my numerous publications on pudendal neuralgia
Special Thanks
Many people’s hard work and knowledge led to the development of transgluteal pudendal decompression surgery, the way I perform this procedure today. I would like to take this opportunity to thank Professor Roger Robert, Professor Oskar Aszman, Dr. Jamie Balducci, Dr. Jacek Bendek, Dr. Mario Castellanos, Dr. May Nour, Cindy Love, and many others.
I want to say a big thank you on behalf of my patients, whom I was able to help with the pain.
Pudendal Neuralgia and Associated Conditions
Here are some of the associated conditions with pudendal neuralgia you should be aware of:
1. Piriformis Syndrome
Piriformis syndrome is a neuromuscular disorder in which the piriformis muscle, located in the buttock region, compresses or irritates the sciatic nerve. This condition may coexist or be confused with pudendal neuralgia, as the pudendal nerve and sciatic nerve are in close proximity anatomically.
Patients with piriformis syndrome often present with pain, tingling, or numbness along the distribution of the sciatic nerve, typically affecting the buttocks and extending down the leg. Treatment usually focuses on addressing the underlying muscle tightness or dysfunction through physical therapy, stretching exercises, anti-inflammatory medications, and, in refractory cases, injections or surgery.
2. Interstitial Cystitis
Interstitial cystitis (IC), also known as bladder pain syndrome, is a chronic, painful bladder condition characterized by pain and pressure in the bladder area, along with a frequent urge to urinate. The pain associated with IC can be debilitating and can significantly impact the quality of life.
Pudendal neuralgia might be connected to interstitial cystitis due to the proximity of the pudendal nerve to the bladder and pelvic floor muscles, which influences the bladder’s sensation and function. Management of interstitial cystitis often involves multimodal strategies, including dietary modifications, physical therapy, medications to reduce bladder pain and inflammation, and sometimes surgical interventions.
3. Vulvodynia
Vulvodynia is a chronic pain condition affecting the vulvar area in women and is often described as burning, stinging, itching, or rawness. The symptoms of pudendal neuralgia and vulvodynia can sometimes be the same. This is because the pudendal nerve supplies feeling to the vulvar area.
There are many things that can cause vulvodynia, including hormonal, genetic, and inflammatory factors. It can be hard to treat. Treatment strategies are typically multimodal, including topical medications, oral pain relievers, pelvic floor physical therapy, cognitive-behavioral therapy, and, in some cases, surgery to decompress the pudendal nerve.
4. Prostatitis
Prostatitis refers to the inflammation or infection of the prostate gland, predominantly seen in men, and is characterized by discomfort, pain, urinary tract symptoms, and sexual dysfunction. Pudendal neuralgia might be interrelated with prostatitis due to the anatomical pathways of the pudendal nerve in proximity to the prostate gland, impacting sensation and pain in the region.
Prostatitis can be caused by bacteria or something else. Depending on the cause, antibiotics, anti-inflammatory drugs, alpha-blockers, and physical therapy for the pelvic floor may help ease the symptoms.
Even though these conditions are different, they may share some symptoms, pathophysiology, and anatomical links with pudendal neuralgia, which makes diagnosis and treatment more difficult. A comprehensive and multidisciplinary approach to evaluating and treating these conditions is crucial for addressing the intricate and multifaceted nature of pelvic pain syndromes.
Pelvic Pain Frequently Asked Questions:
Here are some frequently asked questions that may help you greatly:
-
What is Pelvic Pain?
Pelvic pain in women is a common symptom that accounts for up to 30% of visits to a gynecologist, yet it is thought that close to 70% of cases of pelvic pain are not of a gynecological origin. Chronic pelvic pain is defined as pain that has been present for six months or longer, is localized to the pelvis, and is severe enough to cause functional disability requiring treatment. It is estimated that chronic pelvic pain affects 15% of women in the United States sometime during their lifetime.
Yet, almost 60% of those patients do not have a proper diagnosis (and therefore no treatment). This is because this pain usually spans more than one specialty, and treatment requires physicians specifically trained in chronic pelvic pain. Those statistics are even more staggering because over 20% of women with pelvic pain miss work, close to 50% feel depressed, and in 90% of women, it affects their sexual life.
Pain during or a complete inability to have intercourse significantly affects personal relations between the patient and her partner and further adds to suffering. Despite the fact that chronic pelvic pain in women is more common than coronary artery disease, asthma, or migraine headaches, very few physicians specialize in its treatment.
Pain is often blamed on psychological issues, and patients are often referred to a mental health provider instead of getting treatment for their true, existing disease.
-
What Conditions Cause Pelvic Pain?
Multiple conditions may cause pelvic pain, often coexisting in one patient. Some of the more common conditions are:
- Endometriosis
- Interstitial cystitis/bladder pain syndrome
- Irritable bowel syndrome
- Spastic pelvic floor syndrome
- Adhesions in the pelvis and abdomen
- Pelvic congestion syndrome
- Pelvic nerve neuralgias
- Pain caused by pelvic mesh
The Arizona Center for Chronic Pelvic Pain offers comprehensive treatment for those and many other conditions causing pelvic pain.
-
What is Pudendal Neuralgia?
Pudendal neuralgia is a relatively unknown cause of severe pelvic pain.
In my practice, I define it as pain located in the area of innervation of the pudendal nerve. Pudendal nerve entrapment is an impingement of the pudendal nerve due to scar tissue, surgical supplies, or mesh.
Therefore, pudendal nerve entrapment is one cause of pudendal neuralgia. However, other causes, such as inflammation, spasms of the surrounding muscles, or other nerve diseases, may also cause pain.
-
What is Pudendal Neuralgia for Men?
Pudendal neuralgia is defined as pain in the area of innervation of the pudendal nerve. In men, the areas affected can be the penis, scrotum, perineum, and rectum. Pudendal nerve entrapment is described as compression of the pudendal nerve from ligaments, scar tissue, or surgical materials, which leads to pudendal neuralgia.
Some patients with pudendal nerve entrapment experience burning pain, but others may have a sensation of numbness. It may be present on one or both sides, and some patients experience problems with erection and pain with ejaculation. Penile numbness is one of the more frequent signs of pudendal neuralgia in men.
Conclusion
Managing Pudendal Neuralgia through transgluteal nerve decompression surgery can be a significant step towards reclaiming your life from chronic pain. By understanding the pre- and post-surgery expectations, you can better prepare for a smooth recovery journey.
Remember, the dedicated team led by Dr. Hibner is committed to supporting you every step of the way, ensuring that you receive the highest quality care and personalized treatment. Your path to relief and improved quality of life starts here.
Read More: How Do You Know If You Have Pelvic Floor Dysfunction?
Pudendal Nerve Block
Pudendal Neuralgia in Men
Pudendal neuralgia is defined as pain in the area of innervation of the pudendal nerve. In men, areas affected can be the penis, scrotum, perineum, and rectum. Pudendal nerve entrapment is described as compression of the pudendal nerve from ligaments, scar tissue, or surgical materials which leads to pudendal neuralgia. Some patients with pudendal nerve entrapment experience burning pain but others may have the sensation of numbness. It may be present on one or both sides and some patients experience problems with erection and pain with ejaculation. Penile numbness is one of the frequent signs of pudendal neuralgia in men.
Pudendal nerve entrapment is less common in men than in women and the exact incidence is not known. It is usually related to a traumatic or painful event in the pelvis, penis, scrotum, or anus. It has also been noted in men who masturbate excessively or who insert objects in their rectum. Pain or numbing sensation may occur after one significant trauma or multiple repetitive smaller traumatic events. An example of repetitive smaller trauma is bike riding where a narrow bicycle seat may crush the nerve against ischial tuberosities (sitz bones).

The Pudendal Nerve in Men
Pudendal neuralgia is the pain that a patient feels in the area of innervation of the Sciatic nerve, dorsal nerve, and pudendal nerve. If the patient is a male—the areas affected can be the penis, scrotum, perineum, and rectum (dis colon rectum). If the patient is a female—the pudendal nerve runs from the lower back—along with the pelvic floor muscles to the perineum. This can cause the patient not just perineal pain, but also great pelvic pain—such as chronic pelvic pain and vaginal pain.
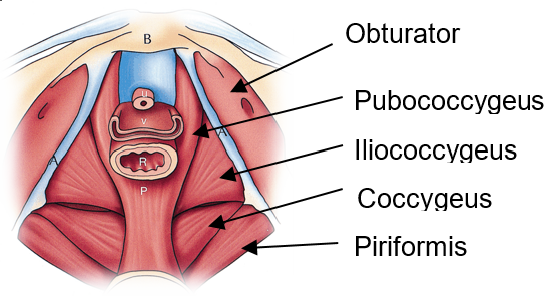
In addition—the pudendal nerve crosses between two muscles. These two muscles are called the coccygeus and the piriformis muscle. Piriformis muscle spasm may also affect the pudendal nerve—controlling our bladder and bowel.
Pudendal neuralgia is less common in men compared to women. The perineal pain and pelvic pain—such as chronic pelvic pain and vaginal pain caused by pudendal neuralgia in a female are commonly related to a painful or traumatic event in the sciatic nerve, pelvis, or anus. While for males—their pudendal neuralgia or the dis colon rectum—is related to painful or traumatic events in the penis, scrotum, anus, or the dorsal nerve.
Symptoms of Pudendal Nerve Involvement
There are some areas along the pudendal nerve’s path (pudendal canal)—where it can be squeezed by other structures—which causes it to become irritated. When the pudendal canal is compressed—that is when pelvic pain and chronic pain in the pelvic area happen.
The pain signal that a patient with pudendal neuralgia is usually described as stabbing and burning or chronic pain in the pelvis. Sometimes—the pain signal can be a tingling sensation or numbness. A pain signal can be worsened by any activity—involving bending your hip—such as squatting or sitting down for too long.
For pain relief—aside from injection with a numbing medicine—the patient can try standing or lying down. There are also some cases where sitting on the toilet gives pain relief to the patient. Since the perineum nerve has so many functions—pressure on the perineum nerve may contribute to a similar pain signal such as— erectile dysfunction, or the pain during ejaculation or urination—as well as—urinary urgency or frequency, bowel or bladder incontinence—and the like.
If any pain medicine doesn’t give any pain relief anymore—then it is the best idea to call a doctor right away. Pain medicine should be able to give pain relief to the patient. Otherwise—pudendal nerve blocks might be necessary.
Pudendal Nerve Blocks
Pudendal nerve blocks are historically a common regional anesthesia technique or also known as the local anesthetic technique. This local anesthetic technique provides perineal anesthesia during an obstetric procedure—such as vaginal birth during the second phase of labor, vaginal repairs—as well as—anorectal surgeries—which include hemorrhoidectomies.
Pudendal nerve blocks are less commonly utilized local anesthetic techniques to provide anesthesia for urological procedures. Nevertheless—this local anesthetic technique is very safe and effective for the patient. The pudendal nerve blocks are used in comforting pain associated with pudendal neuralgia.
Pudendal nerve blocks are more helpful than pain medicine in evaluating—as well as—managing both pelvic and groin pain around the anus, perineum, and genitals. A pain physician gives an injection with numbing medicine with a needle placement on the pudendal artery to determine what is causing your pain.
A pain physician just doesn’t give out an injection with a numbing medicine injected anywhere on your body. A proper needle placement—specifically on the pudendal artery is necessary. Pudendal nerve blocks can be executed via a perirectal approach with the use of a nerve stimulator. A nerve stimulator can stimulate contractions of the outer anal sphincter
The aim of pudendal nerve blocks is to block the nerve as it enters the lesser sciatic foramen—1 cm inferior and a medial comparative to the extension of the sacrospinous ligament to the ischial spine. The sacrospinous ligament is a very thin ligament that is attached to the ischial spine. On the other hand—the sacrotuberous ligament is a stabilizer of the sacroiliac joint. The sacrotuberous ligament also connects the bony pelvis to the vertebral column.
What Conditions Can Pudendal Nerve Blocks Treat?
A pudendal nerve block is used in treating conditions characterized by symptoms of genital/rectal pain (pudendal neuralgia)—which is caused by pudendal nerve entrapment while passing through the pelvic region. It may also become inflamed caused by local trauma—including stretch injury. However—the most common for its inflammation is due to skin-tight clothing, pregnancy, weight gain—or obesity.
How is it Performed?
A team of health professionals will help the patient to be in the proper position to make sure the procedure is done properly and can be completed with the smallest amount of discomfort for the patient. The patient’s skin is cleansed using a sterilizing solution (chlorhexidine). Next—a local anesthetic medication will be given to numb the skin. To find the target—fluoroscopy (x-ray) or ultrasound is done next.
A very thin needle is then directed to the desired location. Then—a local anesthetic and/or steroids are injected. During the entire process—the patient will be constantly monitored by a team of health professionals. A small badge is then placed on the skin after the injection. The patient will be given time after the procedure to ensure that the patient feels fine and is not experiencing and side-effects before leaving the clinic/hospital.
What Kind of Medication is Injected?
The medication inside the injection includes a combination of anesthetic ( bupivacaine or lidocaine) and steroid (dexamethasone, cortisone, or Kenalog). The local anesthetic will be the one responsible for the immediate relief—while the steroid is used to supply more long-term relief.
Does the Entire Procedure Hurt?
The procedure is normally well-tolerated. The most common and uncomfortable part of the procedure is a localized burning sensation from the anesthetic. During the procedure—patients often experience a pressure sensation—which typically resolves within a few minutes. The patient may also feel a minor soreness for a week after the procedure—which is totally normal.
How Long Does Usually the Procedure Take?
The procedure normally takes about 15 minutes. We advise patients to arrive at the hospital/clinic 1 hour prior to allow pre and post-procedural protocols.
For more details on pudendal neuralgia, you may refer to the page on pudendal neuralgia in women. Treatment of pudendal neuralgia in men is similar to treatment in women and surgical decompression of the pudendal nerve (transgluteal pudendal neurolysis) is also done in a similar manner since the anatomy of the nerve in men and women is virtually identical.
If you or anyone you know experiences pudendal pain, contact our office at 480 599-9682 or email [email protected] to learn about available treatments.
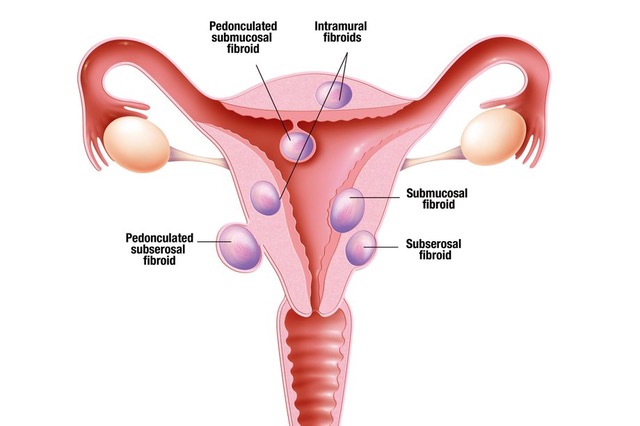
Endometriosis is a condition in which the tissue that normally is present inside the cavity of the uterus, called endometrium, starts growing on the pelvic walls, ovaries, fallopian tubes, bladder, bowels and occasionally pelvic nerves. Despite extensive research it is unclear how patients get endometriosis. There are multiple theories attempting to explain the etiology of this disease. One of the most popular, called Sampson’s theory, states that endometrial cells travel to the pelvis through the fallopian tubes with menstrual blood. Those cells then implant on the pelvic organs, ovaries, fallopian tubes, bowel, bladder and pelvic side walls. The second theory called Myers theory of coelomic metaplasia states that cells that have a potential of becoming endometriosis are already present in the peritoneal lining of the pelvis. Those cells become activated due to environmental or hormonal factors then turn into endometriosis. Unfortunately, neither one of those theories fully explains all the cases of this disease which means that endometriosis may form in several different pathways (may be multifactorial).

Endometriosis implant on the abdominal wall. Bowel on the bottom.
Approximately 10% of women have endometriosis but only half will experience pelvic pain due to this condition. It may be present in about 70% of patients with pelvic pain, and about a third of patients who are undergoing laparoscopy for pain are found to have endometriosis. In patients who have laparoscopy for other reasons than pain 5% has endometriosis. Endometriosis may also lead to infertility which occurs in about 30% to 50% of patients with this condition. The rate of infertility in patients with endometriosis is 2 to 3 times higher than in general population.
Endometriosis is inheritable condition. Children and siblings of people with endometriosis are six times more likely to have this condition themselves. It is not known which genes are responsible for inheritance of endometriosis, but it appears that low level of progesterone hormone or progesterone receptor defect may increase the risk of this condition.
The most common symptom of endometriosis are painful menstrual periods. They occur in approximately two thirds of all the patients with this disease. Those painful periods usually start at the time of the first menstrual period (menarche) and with time get progressively worse. Eventually the pain is not only present during menstrual period but becomes continuous. Patients also experience pain with intercourse, urination, bowel movement and physical activity. Pain in endometriosis is mostly caused by uterine cramping but also cramping of the muscles of the pelvis and abdomen. Irritation of pelvic nerve endings and release of inflammatory substances is also responsible for the pain.
The only way to diagnose endometriosis is to perform surgery (laparoscopy or robotic laparoscopy) and visually confirme the presence of endometriosis implants. Because some conditions may resemble endometriosis, I strongly believe that pelvic lesions which look like endometriosis need to be removed and sent to pathology for microscopic confirmation.
Treatment of endometriosis may be medical or surgical. Medical treatment of endometriosis entails the use of medications which lower the levels of estrogens. Those medications may be effective, but they usually have side effects such as hot flashes, irritability, vaginal dryness and loss of libido. They generally mimic the symptoms that older patient would experience during menopause. Also, because of significant risk of osteoporosis, those medications should not be used for prolonged time. Unfortunately, when those medications are discontinued, endometriosis simply comes back. Research shows that medical treatment of endometriosis with anti-estrogen medications may be beneficial in mild form of endometriosis; in more severe cases they are not effective.
Surgical resection of endometriosis using robotic assisted laparoscopy or in some cases simple laparoscopy is the best treatment for this condition. Resection of endometriosis as opposed to ablation of endometriosis allows for much more precise removal of all the lesions minimizing the risk to vital pelvic and abdominal organs. This procedure, because of the complexity of pelvic anatomy, should be done by trained and experienced surgeon. Since endometriosis often involves bowels, bladder, diaphragm or other or abdominal/pelvic organ it is important that the surgeon is adequately trained to operate not only on reproductive organs but also on urinary and gastrointestinal systems. When lesions presumed to be endometriosis are resected, they should be then sent to the pathology to confirm that they are indeed endometriosis. There is ample research which shows that there are lesions appearing to be endometriosis which are not, and conversely endometriosis may sometimes appear like normal healthy tissue. Patients with severe endometriosis often develop endometriosis in the ovary. It is called an endometrioma. Endometriomas may cause significant pain but also are source of infertility. It is extremely important that surgery to remove endometrioma is done by a very experienced surgeon to preserve as much of a healthy ovary as possible for future fertility and hormone production.
Ovarian endometrioma (bottom of the picture with da Vinci robot instrument pressing on it). Uterus on top of the picture
Surgical removal of endometriosis is successful in treatment of pelvic pain related to endometriosis. One of the most comprehensive studies demonstrated that patients who undergo surgical removal of endometriosis are 10 times less likely to have pain than those who just had diagnostic laparoscopy (surgery to look, without removing any endometriotic lesions). After surgical resection of endometriosis patients usually experience a long pain free period, but endometriosis will most likely return. Because we do not know how endometriosis happens in the first place, we do not know how to prevent it from re-occurring. In some cases (endometriosis in the ovary) birth control pills may delay the return of endometrioma, but in most of the cases birth control pills do not prevent or delay a relapse. A large study of over 850 women have shown that within five years from resection of endometriosis approximately half of the patients will have a reoccurrence of pain requiring another surgery.
In patients with endometriosis who are done with childbearing hysterectomy may be a good treatment option. Hysterectomy by itself does not prevent endometriosis from coming back, but because pain in patients with endometriosis is often from cramping of the uterus, it may prevent the reoccurrence of pain. In the study mentioned previously in seven years from the initial surgery 23% of patients who underwent hysterectomy had another surgery for endometriosis but only 8.3% of patients that had hysterectomy and ovaries removed needed another procedure.

Endometriosis on the diaphragm. Bottom of the picture – liver. Implants of endometriosis on the diaphragm fulgurated (coagulated) with argon beam coagulator.
Patient undergoing surgery for endometriosis may benefit from additional procedures in order to decrease pain. One of those procedures is presacral neurectomy. Presacral neurectomy is a procedure in which one of the nerves in the pelvis responsible for transmitting cramping sensation may be severed decreasing that sensation. Multiple studies have shown that patients with endometriosis undergoing presacral neurectomy have decreased pain (86% of patients are pain free one year from resection of endometriosis and presacral neurectomy versus 57% who just had resection of endometriosis). Presacral neurectomy is done in close proximity to very large pelvic veins (vena cava) and it should only be performed by very experienced surgeons.
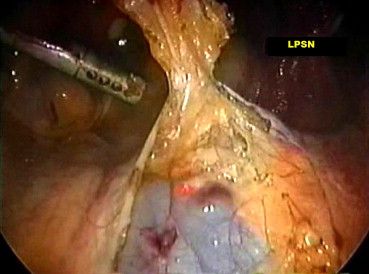
Presacral neurectomy with visible vena cava
One of the most important concepts in treatment of endometriosis is that it coexists with other pain causing conditions in the pelvis. For that reason, endometriosis has been called by some an “evil quadruplet”. The other three are spasm of the pelvic floor muscles, painful bladder syndrome (interstitial cystitis) and irritable bowel syndrome. When suffering from endometriosis it is very important to be treated by a physician who is not only trained and complicated resection of endometriosis but also can address those other conditions. Surgical resection of endometriosis without treatment of coexisting conditions may not bring the desired effects.
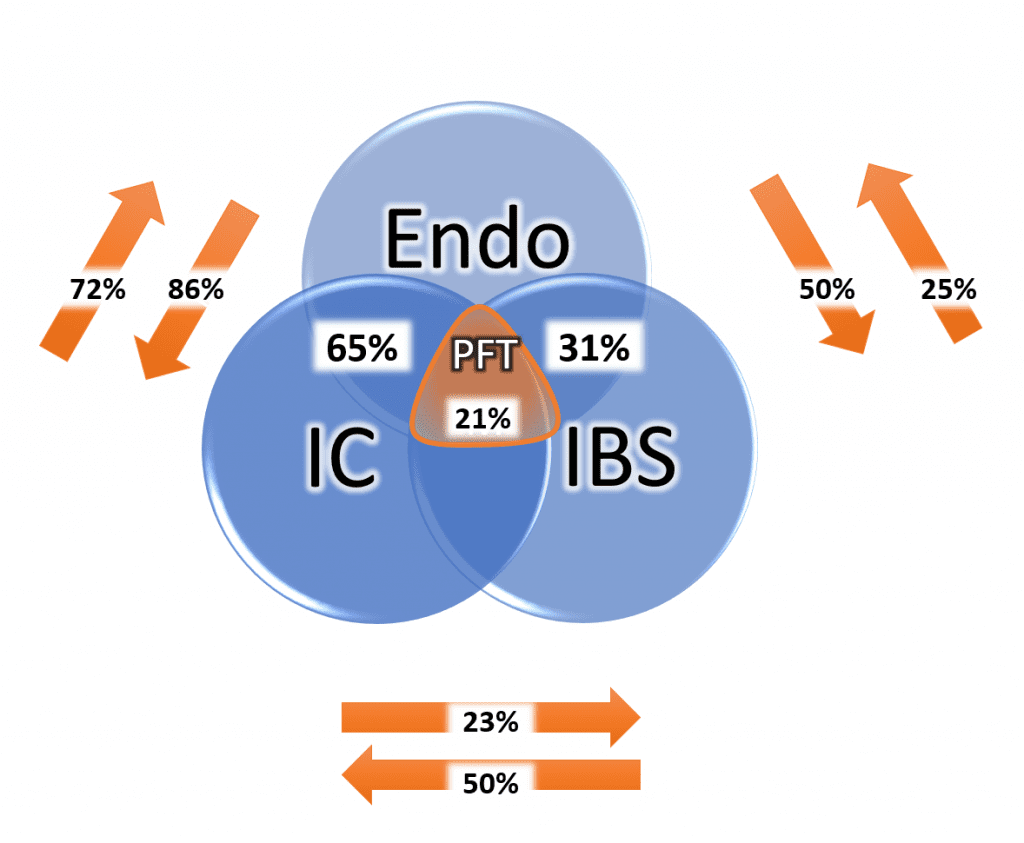
Conditions that coexist with endometriosis (IC – interstitial cystitis, IBS – irritable bowel syndrome, PFT – pelvic floor tension)
If you or anyone you know suffers from endometriosis, contact our office at 480 599-9682 or [email protected] to learn more about available treatments.
Robotic resection of mild endometriosis
Robotic resection of moderate endometriosis
Robotic resection of severe endometriosis and endometrioma
Robotic resection of diaphragm endometriosis
Presacral neurectomy
With aging, childbirth and changes in hormonal status over 50% of women will develop urinary incontinence and prolapse. Those diseases of pelvic floor may be treated non-surgically and surgically. For many years pelvic floor surgeries surgeries were preformed using patients own tissue (native tissue repair), but in 1996 first polypropylene pelvic mesh for treatment of stress urinary incontinence was introduced. It quickly replaced traditional surgical procedures and mesh based procedures became the mainstream treatment for stress urinary incontinence in women. In 2004, mesh for treatment of pelvic organ prolapse was introduced and soon after FDA started receiving information of patients who have developed problems after this surgery. In 2008 FDA issued the first warning regarding the dangers of pelvic mesh; in 2016 pelvic mesh was reclassified as type class III device requiring extensive research before brining devices to the market and in 2019 polypropylene mesh for pelvic organ prolapse was taken off the marked altogether. Polypropylene mesh used in retropubic and transobturator slings continues to be used for treatment of stress urinary incontinence.
Many patients who underwent implantation of polypropylene mesh either for incontinence or prolapse are satisfied with the procedure and do not have any complications. When complication occur, they may range from transient discomfort, to more significant complication of erosion, to absolutely debilitating neuropathic pelvic pain. Some patients also develop significant autoimmune reaction to mesh, which may add to the devastating pain they already experience.
Severe neuropathic pain
Even though severe pain after mesh implantation is rare, when it happens can be completly incapacitating to the patient. This pain may be caused by muscle spasm, nerve injury, inflammation, scarring or foreign body reaction.
Direct nerve injury is one of the most serious complications of mesh implantation. This injury may occur with mesh kits that were designed to attach to, or pierce through the sacrospinous ligament. Anatomically pudendal nerve runs behind the sacrospinous ligament, so any mesh that attaches to this ligament is at risk of injuring the nerve. Mesh kits that attach to the sacrospinous ligament include Prolift, Avulta, Pinnacle, Uphold and several others. Even though the surgeon is advised to place the mesh at the certain distance from the nerve, the blind placement makes it virtually impossible to know the exact location. Patients who sustain direct injury to the nerve will generally experience immediate and severe pain upon waking up from surgery. This type of injury is a true emergency and mesh needs to be removed as quickly as possible to avoid permanent damage. The surgery does not only involve removal of the mesh, but decompression of the pudendal nerve which has to follow. This procedure, therefore, has to be performed by a surgeon who is very knowledgeable in preforming transgluteal pudendal nerve decompression.
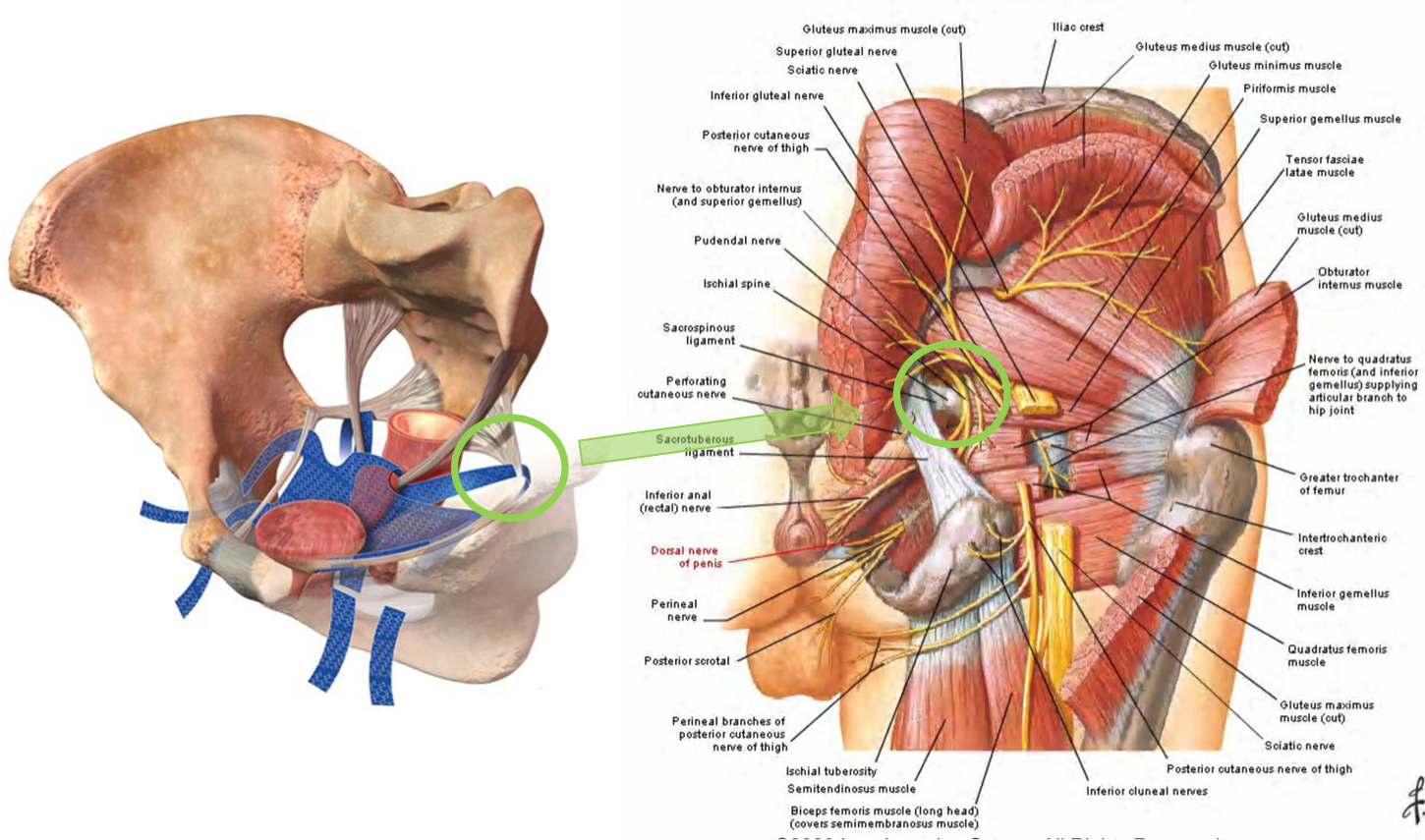
Mesh attaching to the sacrospinous ligament in the proximity of the pudendal nerve
Muscle spasm and delayed nerve injury involves mesh kits that perforate or attach to different pelvic muscles. When woven polypropylene mesh is placed in the muscle it is causing it to spasm through mechanical irritation. With time mesh shrinks adding to even more irritation and spasm. This explains why sometimes pain starts months to years from implantation surgery. Transobturator meshes include products like TVT-O, Monarch, Obtryx, Elevate, Prolift and many, many others. The older transobturator meshes were designed to pierce through several muscles in the groin including obturator internus muscle and exit on the skin of the thigh. In case of those mesh kits, the adductor muscles (muscles that bring legs together) are often affected, so patients experience groin pain with walking and almost any movement of lower extremities.
Transobturator (older type) mesh piercing multiple muscles in the groin
Transobturator mesh (newer type) attaching to the obturator internus membrane/muscle
The newer products are made to attach to obturator internus membrane/muscle without penetrating any other muscles. Those meshes may still mechanically irritate the obturator internus muscle triggering it to spasm. The obturator internus muscle is respo
![]()
![]()

![]()

![]()
![]()
![]()
![]()
Blue arrow shows the approximate location where transobturator mesh pierces obturator internus muscle. Green line shows the approximate course of pudendal nerve within obturator internus muscle (Alcock’s canal-pink). Yellow line shows approximate course of the obturator nerve to the obturator canal
Pudendal nerve runs through the obturator internus muscle through the part known as Alcock’s canal. When obturator internus muscle is spasming it is putting pressure on the pudendal nerve in the Alcock’s canal giving patients symptoms of pudendal neuralgia such as burning pain in the perineum, rectum, clitoris and vagina which is typically worse with sitting.
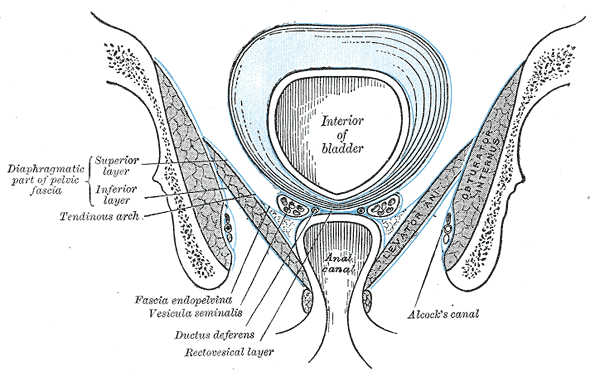
Obturator internus muscle with Alcock’s canal containing pudendal nerve
Groin mesh removal
Those transobturator meshes are also placed in the proximity of the obturator nerve, but rarely cause direct injury to this nerve. They may injure obturator nerve in the indirect mechanism though since the spasming obturator internus muscle is putting pressure on the obturator nerve at the obturator canal. Patients develop symptoms of obturator neuralgia such as groin pain and pain on the inside of the thigh which is worse with walking.
Groin mesh removal with identification of obturator nerve
Delayed mesh injury also occurs with retropubic meshes. Those meshes pierce through pelvic floor muscles and when they irritate them, they also may cause them to spasm. Spasming pelvic floor muscles also place pressure on pudendal nerves triggering symptoms of pudendal neuralgia.
Retropubic mesh perforating pelvic floor muscles
Robotic removal of mesh
Autoimmune reaction
In my practice close to 50% of patients who have developed pain after mesh placement have also developed new onset autoimmune condition which they did not have prior to the mesh placement. Most common conditions observed were Sjögren syndrome, lupus and Hashimoto’s thyroiditis. Patients often experience unexplained rashes on the legs, arms, muscle aches and fatigue. Symptoms are usually quite debilitating and not amenable to treatment unless mesh is removed. Fortunately, when mesh is completely removed autoimmune symptoms improve
If patient has symptoms of nerve injury (pudendal, obturator or other pelvic nerves) it is of utmost importance that she is treated by a provider who specializes in treating mesh complications, preforms complete mesh removal surgery, but also is knowledgeable in pelvic nerve injury and surgical nerve decompression. Dr. Michael Hibner is the only provider in United States, who is board certified in Female Pelvic Medicine and Reconstructive Surgery (urogynecology) who performs complete mesh removals and specializes in pelvic nerve decompression surgery.
Removal of mesh from pudendal nerve
Dr. Hibner strongly believes that it is the arms of the mesh deeply embedded into the pelvic muscles that have a potential of causing severe pelvic pain. Removing just the vaginal part of the mesh in most of the cases is not going to help with pain. It is the arms that need to be removed in order to help with pain and it may be much more difficult to remove those arms if the vaginal part has been previously removed. It is best to remove the entire mesh in one piece during the same surgery. The complete mesh removal is also very important in patients who have developed autoimmune symptoms after mesh placement. In order to alleviate autoimmune symptoms every piece of polypropylene has to be removed.
If you or someone you know have developed pelvic pain or autoimmune symptoms after mesh placement call our office 480 599-9682 to learn more about available treatments.
Pelvic Floor Spasms
Pelvic Floor Spasms are one of the most common conditions leading to pelvic pain both in women and in men.
This condition is one of the “evil quadruplets” since it tends to co-exist with endometriosis, interstitial cystitis/bladder pain syndrome, and irritable bowel syndrome. The condition is like having a charley horse in the muscles that surround the vagina, urethra, and rectum. There are multiple reasons why this spasm happens.
Most often, it is some other pelvic pain condition that, through complex neural mechanisms, is irritating the pelvic muscle(s). Patients who have chronic pain from endometriosis, chronic pelvic pain syndrome, pelvic floor disorder, or pelvic trauma may develop spasms, which, unless treated, may last for many years. Some patients may also develop spasms after psychological trauma or even without any significant precipitating event.
Most commonly, patients with pelvic floor spasm(s) will experience pain during intercourse, urination, and bowel movement, as well as any physical activity. Generally, this pain persists from hours to days after sexual function or sexual intercourse. It may also persist after urination or bowel movement. Patients with muscle spasms may also have trouble starting the urine flow or difficulty in completely emptying the bladder. Because of that incomplete emptying, they often get up at night multiple times to urinate.
Pelvic floor spasm(s) may be easily identified during a physical exam or women’s health exam by a trained pelvic pain physician or pelvic floor physical therapist. Treatment consists of pelvic floor physical therapy and muscle relaxants.
The majority of patients are helped by those two modalities. In cases where muscle spasm is not relieved by pelvic floor physical therapy and muscle relaxants, botulinum toxin injections to the pelvic floor may be necessary. Treatment of the underlying pain is also very important.
In cases where pelvic floor muscle spasms developed because of other symptoms such as endometriosis, treatment of that underlying condition is very important. If someone has developed pelvic floor muscle spasm after placement of pelvic mesh, the mesh has to be addressed first before addressing muscle spasm.
At Arizona Center for Chronic Pelvic Pain, we work with physical therapists in the Phoenix area and throughout the United States. We strongly believe that pelvic floor physical therapy is the most important part of relieving pelvic muscle spasm(s). In most cases, we will be able to recommend a physical therapist in your area or provide you with resources to find one. Strengthening weak pelvic floor muscles through pelvic floor exercises is critical.
Muscle relaxants are usually used in the form of a vaginal or rectal suppository and seem to be more effective than oral medications. Different formulations of suppositories exist, and they will be discussed with you during the visit. Botulinum toxin A (BotoxÒ) injections are offered to patients when physical therapy and suppositories fail. Those injections relieve muscle spasms and pain in the great majority of patients, but they may need to be repeated every few months. Because those injections are painful, they should always be done under sedation.
If you have difficulty finding a pelvic floor physical therapist in your area, please contact our office. We collaborate with therapists around the country, and we may be able to help you find one in your area. You can also visit the page of the International Pelvic Pain Society, the Women’s Section of the American Physical Therapy Association, or Herman and Wallace Pelvic Rehabilitation Institute to find a provider in your area.
If you or someone you know is experiencing pain related to pelvic floor muscle spasms contact our office at 480 599-9682 or [email protected] to learn more about available treatments.
What to expect after BotoxÒ injection?
- BotoxÒ injections to pelvic floor muscles are almost always done in conjunction with pudendal nerve(s) block. The block is done to decrease pain after the procedure. When you wake up from the sedation after BotoxÒ injection, you will feel numbness in the pelvis, and you may have numbness in one or both of your legs. Numbness is completely normal and will disappear when the local anesthetic wears off.
- If you have numbness in your legs, you should avoid walking until the numbness goes away. You should have someone help you walk the first time you get up after the procedure.
- After the procedure, you may have difficulty emptying your bladder. Pelvic floor muscles are irritated immediately after the injection, and some patients may need a urinary catheter for a few days. Difficulty emptying the bladder goes away after BotoxÒ starts working and relaxes pelvic floor muscles.
- You may experience vaginal bleeding for 2-3 days after the procedure. It is completely normal, as long as the amount of bleeding is less than the menstrual period.
- After the local anesthetic wears off your pain may come back, and it may come back worse than it was before the procedure. This is because muscles are irritated from the injection. BotoxÒ starts working about one week after the procedure, but it may take 10-14 days to feel the relief of pain.
- It is very important to continue physical therapy after BotoxÒ Botulinum toxin by itself does not permanently cure muscle spasm, but it allows physical therapist to work more aggressively on your pelvic floor muscles.
- BotoxÒ wears off approximately 3-4 months after the injection. Some patients will not go back into spasm, but most will need a repeat injection. If you or your physical therapist feel your muscle spasm is returning, call our office to be scheduled for a repeat procedure.
Pelvic Floor Spasms
Pelvic floor dysfunction is a complex condition that encompasses a wide range of symptoms and abnormalities related to the pelvic floor. The pelvic floor, a supportive sling of muscles spanning the base of the pelvis, plays a pivotal role in the proper function of pelvic organs and the pelvic region. Dysfunction in this area can manifest in various ways, including hypertonic pelvic floor dysfunction, where the muscles of the pelvic floor remain persistently contracted, leading to pelvic muscle spasm or pelvic floor muscle spasm. This involuntary muscle tension can be distributed unevenly across the pelvic area, resulting in localized or generalized pelvic pain. Certain conditions like levator syndrome, caused by spasms in the levator ani muscle, and proctalgia fugax, an episodic, intense pain in the rectal area, are specific types of pelvic pain associated with pelvic floor muscle dysfunction. This hypertonicity can also negatively impact sexual function, with conditions like vaginismus, where the muscle spasm prevents or makes sexual intercourse painful. Moreover, disturbances in the pudendal nerve, which runs through the pelvic floor, can exacerbate or even initiate muscle spasms, thereby perpetuating chronic pain.
Many individuals suffering from pelvic floor disorders, including pelvic floor muscle spasms, experience challenges in their daily lives beyond pain. For instance, urinary incontinence and fecal incontinence, the involuntary loss of urine or stool, respectively, can result from abnormal muscle behavior or weakened connective tissue supporting the pelvic organs. Pelvic organ prolapse, where pelvic organs descend due to weakened support structures, is another consequence of pelvic floor disorder. Beyond these physical manifestations, the chronic pain and incontinence can significantly hinder one’s quality of life. Fortunately, therapeutic interventions such as pelvic floor physical therapy, overseen by a trained physical therapist, offer targeted exercises to strengthen, relax, and improve the coordination of the pelvic floor muscles. In more severe cases, muscle relaxants may be prescribed to alleviate persistent pelvic floor muscle spasms. Through a comprehensive approach addressing both the physical and emotional ramifications, individuals with pelvic floor dysfunction can find relief and reclaim control over their pelvic health.
Pelvic floor spasms, a subset of the broader condition known as pelvic floor dysfunction, refer to the involuntary and persistent contraction of the muscles located in the pelvic region. The pelvic floor musculature, comprising a complex web of muscles, ligaments, and connective tissue, plays a pivotal role in supporting the bladder, rectum, and other pelvic organs. When these muscles undergo undue tension or muscle spasms, it can lead to a variety of uncomfortable and sometimes painful symptoms. Patients might experience challenges during sexual intercourse due to muscle tension, leading to compromised sexual health and function. Additionally, an overactive bladder, urinary incontinence, and even symptoms similar to irritable bowel syndrome can manifest when the pelvic floor muscles are in persistent spasm. As these muscles are closely associated with the ani muscle, any dysfunction in this region can severely impact daily activities and overall well-being.
Addressing Pelvic Floor Spasms
To address pelvic floor spasms, it’s vital first to identify the root cause of the dysfunction. For some, the muscle tension might be a reaction to conditions like pelvic organ prolapse, where the pelvic organs descend due to weakened support structures. For others, it might be a standalone issue. Once identified, tailored interventions can be suggested. Pelvic floor exercises, often guided by trained physical therapists, aim at both strengthening and relaxing the pelvic floor muscles. This ensures that they function optimally, providing the necessary support without being perpetually tense. Manual therapy can also be a beneficial intervention, where therapists use hands-on techniques to release muscle tension and alleviate spasms. In more severe cases, muscle relaxants might be prescribed to combat persistent pelvic floor muscle dysfunction. An integrated approach, focusing on both symptomatic relief and addressing the underlying cause, ensures that individuals can regain control over their pelvic health, ensuring a balanced and functional pelvic area.
Interstitial cystitis (bladder pain syndrome) is a condition which is characterized by the bladder pain during the filling phase. Patients usually complain of pain as the bladder gets full and because of that they urinate frequently to avoid pain sensation. Patients also complain of urgency (got to go sensation) and getting up at night multiple times to urinate. There is always pain with intercourse especially in positions where bladder is directly irritated by the partner’s penis. Patients often have pain outside the bladder, in the vulva, lower back and abdomen. Certain foods and drinks, especially acidic, spicy, containing coughing or alcohol are known to trigger pain and urgency in patients with bladder pain syndrome. Drinks include coffee and tea (both caffeinated and decaffeinated), soda, alcohol, citrus juices, and cranberry juice. Fruits which acidified urine are lemons, limes, oranges, grapefruit, pineapple, kiwi fruit as well as vegetables such as chili peppers, onions, sauerkraut, tomato products and pickles worsen interstitial cystitis symptoms. Processed cheese, dark chocolate and yogurt are also known to aggravate the bladder.
Pathophysiology of interstitial cystitis is not known, and many different theories have been proposed to explain this disease. They range from an infection which is not easily detectable by available techniques to autoimmune process to pelvic floor muscle spasm and incomplete emptying. This lack of understanding of how patients get interstitial cystitis makes the treatment of this condition much more difficult.
There is also a big disagreement among providers on how to diagnose interstitial cystitis, and most diagnose it based on patient’s symptoms. Additional studies such as urine analysis, urine culture and cystoscopy may be necessary to rule out other conditions that may be adding to bladder pain. Looking for glomerulations on cystoscopy or potassium sensitivity test are not used in modern diagnostic process of interstitial cystitis.
There are multiple available treatments for interstitial cystitis which include diet modifications, relaxation techniques oral medications but one of the most important concepts is treatment of the pelvic floor muscles. Additionally, treatments involving hydrodistention of the bladder may be very beneficial.
If you or someone you know suffers from interstitial cystitis/bladder pain syndrome call our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Pelvic Congestion Syndrome | What conditions are associated with Pelvic Congestion Syndrome?
Varicose Veins or Vein Engorgement
When blood pools in the pelvic vein or ovarian vein, it may result in enlarged veins, causing pain, tenderness, and redness. Varicose veins usually develop in the legs, calves, and feet, but can also occur in the pelvic region, leading to pelvic congestion syndrome.
Deep Vein Thrombosis (DVT)
DVT occurs when a blood clot forms in a deep vein, and this can occur in the pelvis. The clot then restricts blood flow, which in turn causes pain, swelling, and often varicose veins, such as in the left ovarian vein.
Hydro-nephrosis
Compression on the renal vein can affect urine flow and backing up of urine into the left kidney, causing pelvic congestion syndrome symptom. As a result, affected individuals may report chronic pain and frequent urination.
Peripheral Artery Disease (PAD)
Cholesterol and fat can build up in the arteries forming plaque that blocks blood flow. This leads to peripheral artery disease, wherein the reduction of blood flow affects the iliac arteries in the pelvis. Those affected may suffer from pain and cramps. Men may also experience erectile dysfunction.
Who is at Risk for Pelvic Congestion Syndrome?
Since studies have shown a link between pregnancy and pelvic congestion syndrome, women who have given birth are at risk for developing this condition. Women who have had multiple pregnancies (carrying more than one baby, e.g. twins) are even more at risk than those who have had a singleton pregnancy (carrying one baby), as they are more likely to develop pelvic varices or enlarged veins in the pelvic region.
In addition, those who have a history of pelvic congestion syndrome in the family are also at risk. If you are suffering from chronic pelvic pain and believe you might have this condition, get in touch with a qualified healthcare provider like AZCCPP.
Can I manage Pelvic Congestion Syndrome on my own?
While this condition is not fatal, if left undiagnosed or untreated, pelvic congestion syndrome can lead to further health complications like chronic pelvic pain and permanently damaged vein. Only qualified healthcare professionals like our team at AZCCPP can help you manage it properly through treatments such as interventional radiology and ovarian vein embolization.
We strongly advise you to get in touch with us so we can make the right diagnosis and provide the best pelvic congestion syndrome treatment option for your case.
What are Pelvic Varicosities?
Pelvic congestion syndrome is a condition where pelvic veins become engorged and form pelvic varicosities. Pelvic varicosities usually occur during pregnancy and disappear after. In some patients, they remain, causing pelvic congestion syndrome. It may occur after a full-term pregnancy, but also after preterm birth, miscarriage, or even after ectopic pregnancy. The mechanism in which varicosities cause pain is not well understood, but it may be due to stretching of the vein wall, pressure on the surrounding nerves, or changes in tissue pH. Some varicosities occur in the ovarian veins and veins around the uterus but some patients have varicosities in the vulvar area pressing against the nerves innervating the clitoris, urethra, and labia.
Depending on the location of congested veins patients will experience different symptoms. Congestion of ovarian and uterine veins leads to the sensation of heaviness in the pelvis which is worse with sitting and standing for a prolonged time and better with laying down. On top of the sensation of heaviness, there is occasional sharp shooting pain in the lower abdomen usually on the left side lasting several seconds at a time which may occur a few times a day to a few times per week.
Pelvic congestion may be diagnosed on pelvic MRI or ultrasound but the gold standard test for diagnosis is transfundal venogram.
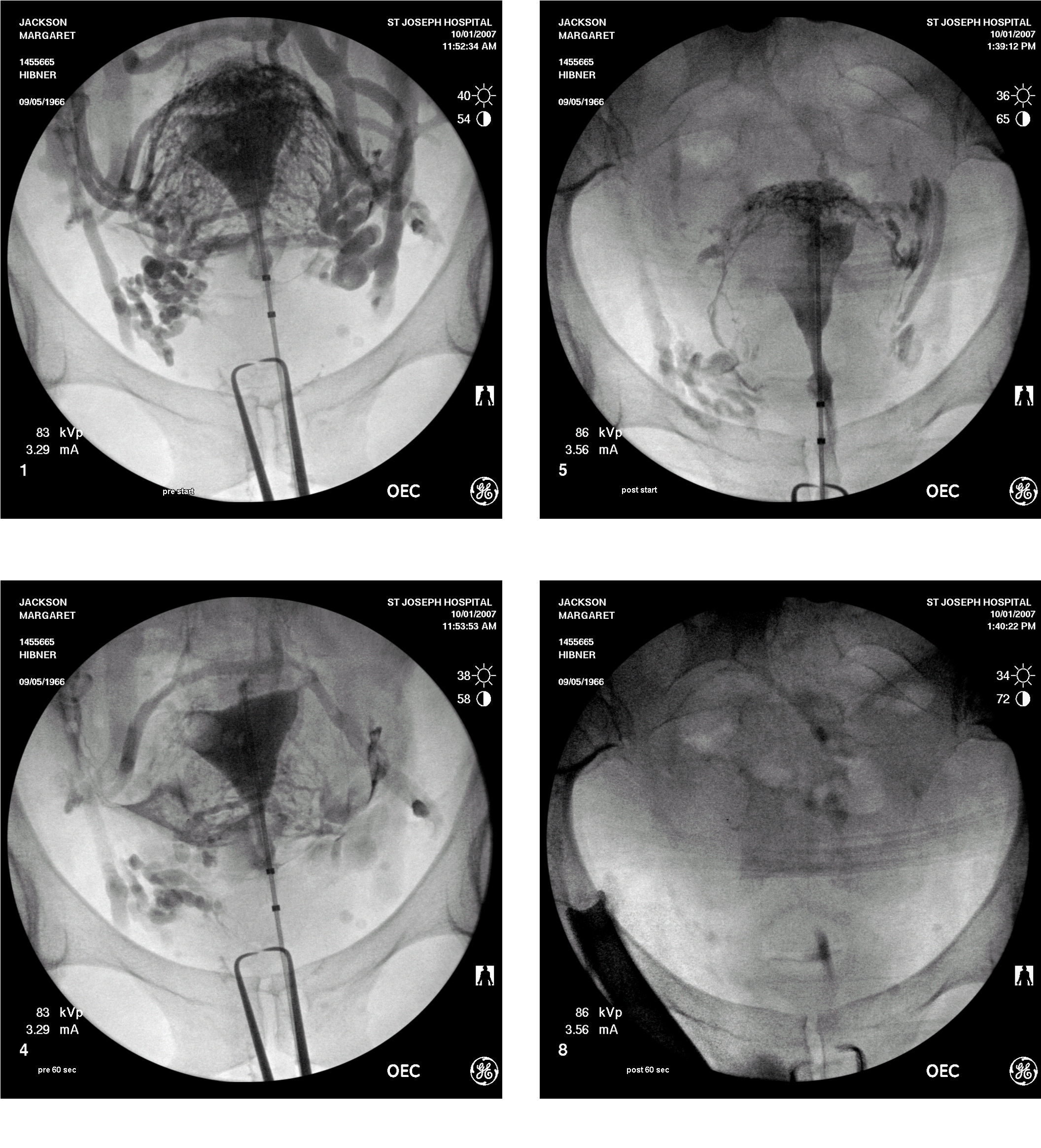
Typical appearance of pelvic congestion syndrome on transfundal venography
Treatment of pelvic congestion may be done by an interventional radiologist who obliterates the congested veins in an attempt to decrease pain. Congested veins may also be closed off surgically by isolating them from the surrounding structures such as nerves and arteries and sealing with a vessel sealing device. An additional benefit of surgical treatment using da Vinci robot over radiological treatment is that surgical treatment of pelvic congestion allows to precisely survey the pelvis and address any other cause of pelvic pain.
Congestion of the veins around the clitoral or perineal branch of the pudendal nerve can only be seen during a special ultrasound examination. This congestion will lead to pain in the clitoris, urethra, and labia and it is worse with sitting and standing. Patients may also experience the sensation of persistent sexual arousal. This type of congestion may be treated by injecting a sclerosing agent into the congested vein in a similar manner as it is done into varicosities in the legs.
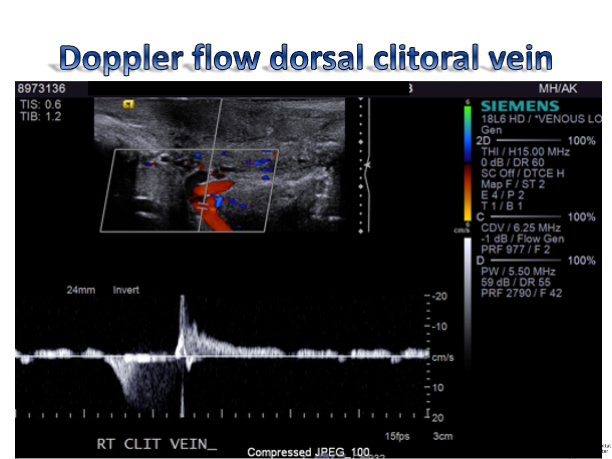
Doppler ultrasound demonstrating congestion in the clitoral vein
What are the Signs and Symptoms of Pelvic Congestion Syndrome?
Again, pelvic congestion syndrome affects everyone differently. It will depend on which pelvic structure the varicose veins are affecting. Here are some signs and symptoms of this condition:
- Your vulva is swollen or you have varicose veins in your genital area.
This happens when pelvis varicose veins go out into the vulva or vagina.
- You have an irritable or painful bladder.
When the pelvic varicose veins push on the bladder, you may feel discomfort or pain when urinating.
- You have hemorrhoids.
Pelvic varicose veins that go into the anus and around the back of the passage may result in bleeding, discomfort, or pain in this area, especially when passing stool.
- You have an irritable bowel.
When the pelvic varicose veins push on the bowel, you may experience symptoms similar to irritable bowel syndrome (IBS): bloating, gas, abdominal pain, cramping, diarrhea, and constipation.
- You experience discomfort or pain during and after sexual intercourse.
This is due to the pelvic varicose veins pushing on the gynecological organs.
- Your pelvic pain worsens during your menstrual cycle.
When the weight of the blood in the veins pushes down on the pelvic floor, you may feel an unusual level of discomfort during your period. You may also experience abnormal bleeding.
- Your pelvic pain worsens throughout the day, especially after physical activities.
Usually, the pain intensifies after sitting or standing for too long, or after physical exercise such as walking, jogging, and lifting weights.
- You feel exhausted.
PCS can be just as draining emotionally as it is physically due to the accompanying
discomfort or pain. Hence, many women claim they also suffer from fatigue and even
mood swings.
Since various conditions exhibit the same signs and symptoms as pelvic congestion syndrome, it is important to consult with a trusted physician for accurate diagnosis and proper treatment.
What Causes Pelvic Congestion Syndrome?
Normally, the arteries send blood from the heart to the rest of the body. Then, the veins send blood from the body back to the heart. This flow is made possible by valves within the veins, which keep the blood from going into reflux or flowing backward.
When the veins become dilated, the valves do not close properly. Reflux then occurs, which leads to pooling of blood within the affected organ–in this case, the pelvis. This results in varicose veins and pelvic congestion syndrome.
While the reason for this condition is unknown, most people who suffer from it are women between the ages 20 and 45 who have had previous pregnancies. One theory suggests that the following can cause pressure within the ovarian veins, leading to vein dilatation:
- Age (particularly during childbearing years)
- Genetics
- Polycystic ovaries
- Retroverted uterus
- Anatomic changes in the pelvic structure due to pregnancy
- Hormonal changes due to pregnancy
- Hormonal dysfunction due to pregnancy
- Weight gain due to pregnancy
- Fluid buildup due to pregnancy
- Increase of blood volume due to pregnancy
- Increase of estrogen due to pregnancy
How Can You Avoid Pelvic Congestion Syndrome?
Since the cause of pelvic congestion syndrome remains unclear, it is not always possible to avoid this condition. However, the risk may be reduced by doing the following:
- Eat a healthy diet
- Exercise regularly
- Quit smoking
- Maintain a healthy weight
- Maintain a healthy body mass index (BMI)
- Wear compression garments during pregnancy
- Wear compression garments on a routine basis after pregnancy
Pelvic Congestion Syndrome in Pregnancy
When a pregnant woman suffers from pelvic congestion syndrome, symptoms usually worsen as the baby grows. The baby’s weight and size exert pressure on the varicose veins of the pelvis, causing great discomfort or pain. The pain may be a dull ache, throbbing, or sharp.
Sitting or standing for a long time can cause the pain to worsen at the end of the day. The best way to relieve it is by lying down. Additionally, every subsequent pregnancy may also worsen the pain.
Outlook
Pelvic Congestion Syndrome may not be fatal, but it can greatly affect your quality of life. For instance, symptoms like hemorrhoids, pelvic pain, and fatigue can take a toll on your physical, mental, and emotional wellbeing.
Fortunately, the symptoms can be minimized and managed with treatments. Your physician might also recommend counseling to help you cope with chronic pain associated with this condition.
To know your treatment options, consult with your doctor.
If you or someone you know has pain that started after pregnancy and has symptoms of pelvic congestion, call our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Adhesions are the scar tissue which forms in the abdominal cavity and pelvis between the loops of the bowel, the bowel and the walls of the pelvis, the pelvic organs and the content of the abdomen. They may range from few areas of fine scar to the very dense obliterated abdominal and pelvic cavity. Adhesions form as a result infections, trauma or previous surgeries. Patients with intra-abdominal and pelvic adhesions generally experience sharp pain which may be more severe with physical activity, rapid movement, especially turning from side to side at night.
There is a disagreement among providers if adhesions cause pain and if removing adhesions relieves pain. In my practice however most of my patient’s significantly benefit from removal of scar tissue. If surgery can be accomplished using minimally invasive techniques such as laparoscopy or robotic assisted laparoscopy the return of adhesions is less likely. Surgical removal of adhesions (adhesiolysis) is not only a compilated and lengthy procedure, but also carries risks which will be discussed with each patient individually.
It is of utmost importance that removal of adhesions (adhesiolysis) is performed by surgeon who is very knowledgeable in pelvic and abdominal anatomy, knowledgeable in bowel, urinary and reproductive surgery as well as in minimally invasive techniques.
If you or someone you know has pelvic or abdominal pain caused by adhesions call our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Pudendal Nerve Entrapment | Understanding the Causes, Symptoms, and Treatment
Pudendal Nerve Entrapment, a condition that affects the pudendal nerve in the pelvic region, can produce chronic pain and interfere with daily activities. This post aims to provide valuable insights into understanding the condition, recognizing its symptoms, diagnosing and treating it, implementing lifestyle modifications, and adopting preventative measures for long-term management.
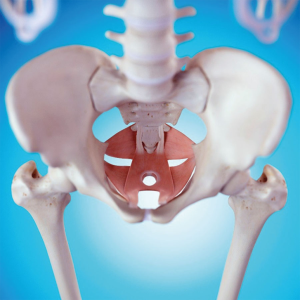
Understanding Pudendal Nerve Entrapment
What is Pudendal Nerve Entrapment?
As mentioned, pudendal nerve entrapment (PNE) is a chronic pain condition caused by irritation or compression of the pudendal nerve. The pudendal nerve is the primary nerve responsible for movement and sensation in the pelvic area, which includes the genitalia, rectum, and bladder. PNE can result in a variety of symptoms, such as:
- Pain in the buttocks, perineum (the area between the genitals and anus), and genitals
- Numbness or tingling in the same areas
- Difficulty with urination or bowel movements
- Pain during sex
- Pain when sitting
Causes and Risk Factors
Although it is not understood what causes PNE, here are some things that can put you at a higher risk of being diagnosed with it:
- Injury to the pudendal nerve during childbirth or surgery
- Repetitive strain injuries, such as from prolonged sitting or cycling
- Structural abnormalities of the pelvis, such as a narrowing of the sacrospinous ligament
- Inflammatory conditions, such as arthritis or endometriosis
- Tumors or cysts in the pelvic region
Common Entrapment Sites
The pudendal nerve can become entrapped in various areas, including:
- The greater sciatic notch, where the nerve exits the pelvis
- The Alcock canal is a tunnel in the pelvis that the nerve passes through
- The pudendal nerve fascia, a sheath of tissue that surrounds the nerve
- The perineal body is a small mass of tissue at the junction of the vagina and anus
Differentiating Pudendal Nerve Entrapment from Other Pelvic Conditions
Diagnosing pudendal nerve entrapment can be challenging because its symptoms often mimic those of other pelvic disorders, such as:
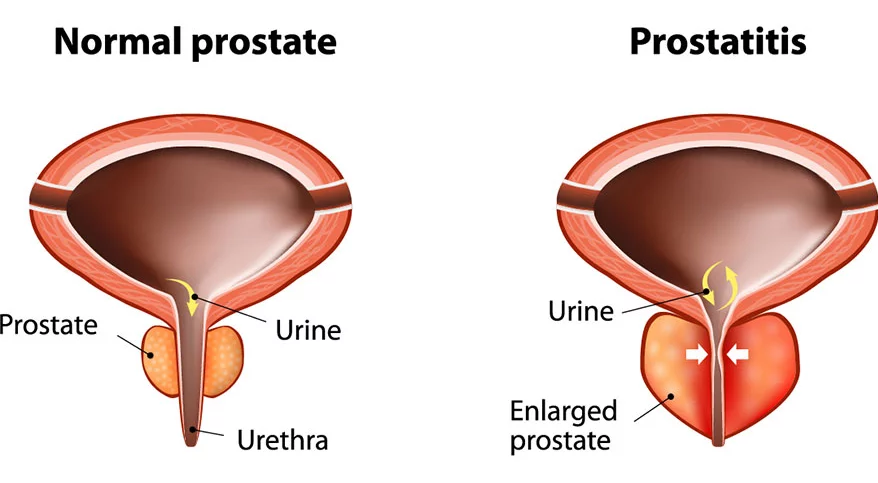
Typically, a clinician will diagnose PNE after conducting a thorough physical examination, reviewing the patient’s medical history, and conducting diagnostic tests like:
- Electromyography (EMG) is a non-invasive technique for gauging muscle electrical activity.
- Nerve conduction velocity (NCV) testing, which measures the speed at which nerve impulses travel
- Pudendal nerve block, which involves injecting a local anesthetic near the pudendal nerve to numb the area and help diagnose PNE
Treatment for Pudendal Nerve Entrapment
Treatment for PNE is patient-specific, as there is no universally effective method. Some potential methods of treatment are:
- Medications, such as anti-inflammatories, pain relievers, or muscle relaxants
- Treatment with physical therapy can aid in the stretching and strengthening of the pelvic muscles.
- Injections of steroids or botulinum toxin into the pudendal nerve
- Surgery, which may be an option for patients who have not responded to other treatments
Those with symptoms consistent with pudendal nerve entrapment should visit a doctor immediately. Your symptoms and overall quality of life may benefit from prompt diagnosis and treatment.
Symptoms of Pudendal Nerve Entrapment
Recognizing the signs of pudendal nerve entrapment is crucial for an accurate diagnosis and prompt treatment. The following are some general warning signs to keep an eye out for. However, individual manifestations may vary:
Chronic Pelvic Pain
Chronic pelvic pain is a classic sign of pudendal nerve entrapment. This discomfort is often described as a dull ache in the pelvic region that has been going on for more than six months.
The discomfort could be restricted to one area or spread to the thighs, lower back, or both. It can make even simple things like sitting, walking, or having sexual relations very uncomfortable.
Pain during Sitting or Prolonged Standing
Sufferers with pudendal nerve entrapment may feel discomfort over prolonged periods of sitting or standing. The soreness in the pelvic region might be made worse by sitting on hard surfaces or for long periods. This symptom can significantly influence one’s ability to work, interact socially, and enjoy life.
Numbness or Tingling in the Genital Area
Pudendal nerve entrapment can cause numbness or tingling in the vaginal area. The external genitalia, perineum, and rectum are all sensory organs that receive input from the pudendal nerve.
Numbness, tingling, or “pins and needles” might result from nerve endings being crushed or entrapped. These feelings can be fleeting or constant, and they have the potential to disrupt sexual performance and general well-being.
Sexual Dysfunction and its Impact
Sexual dysfunction may be severely affected by entrapment of the pudendal nerve. Reduced libido, erectile dysfunction in men, and other forms of pain or discomfort during sexual engagement can affect both men and women.
These symptoms can put a burden on personal relationships and cause mental anguish. When dealing with sexual health difficulties, consulting with a healthcare expert who can provide guidance and appropriate treatment options is essential.
Symptoms of Bowel and Bladder Issues
Bowel and bladder problems are additional symptoms of pudendal nerve entrapment. Some people may have increased frequency, urgency, or incontinence of the urine or bowel systems.
These symptoms can cause severe disruptions in everyday life and must be managed cautiously. These symptoms may point to pudendal nerve involvement and necessitate evaluation by a medical professional.
Diagnosis and Treatment Options
Diagnostic Methods for Pudendal Nerve Entrapment
The key to successful treatment of pudendal nerve entrapment is a correct diagnosis. To diagnose a patient’s illness and come up with an effective treatment plan, medical practitioners use a variety of techniques.
Physical Examination and Medical History
To make an accurate diagnosis, it is necessary to perform both a physical examination and a detailed review of the patient’s medical history. The doctor will talk to you about your symptoms, their length, and what might be causing them. The examination could include the following:
- Testing the patient’s pelvic muscle strength.
- Feeling for pain or stiffness.
- Gauging their sensitivity in the genital area.
Nerve Conduction Studies: Assessing Nerve Function
The health and efficiency of the pudendal nerve are often assessed with a nerve conduction study. This painless examination evaluates how quickly and powerfully electrical impulses travel through a nerve. Healthcare providers can detect anomalies or entrapment of a nerve by testing its conduction ability.
Electromyography (EMG): Measuring Muscle Activity
Electromyography (EMG) is another diagnostic tool that can be used to evaluate muscle function. Needles of varying sizes are inserted into targeted muscles to record the electrical activity during contraction and relaxation. This evaluation helps detect muscle dysfunction or anomalies that could cause a pinched pudendal nerve.
Diagnostic Nerve Blocks: Confirming the Diagnosis
Medical providers may use diagnostic nerve blocks to confirm a diagnosis of pudendal nerve entrapment. A local anesthetic is given close to the pudendal nerve to evaluate the patient’s response and provide temporary pain relief. The pudendal nerve’s involvement in pain creation would be further supported if the pain dramatically improved following the nerve block.
Non-surgical Treatment Options
Medications for Pain Management
The symptoms of pudendal nerve entrapment can often be alleviated with medication. Non-steroidal anti-inflammatory drugs (NSAIDs), neuropathic pain medications, and muscle relaxants are some pain medications that medical experts may give to assist in alleviating pain and enhance daily functioning.
Physical Therapy and Pelvic Floor Exercises
Physical therapy and pelvic floor exercises are frequently suggested as a non-invasive alternative to surgical intervention. A trained physiotherapist can show patients how to do exercises that strengthen and stretch the pelvic muscles while also helping them relax. All around, pelvic stability and function are enhanced, and muscle tension is eased thanks to these workouts.
Nerve Stimulation Techniques: A Promising Approach
Transcutaneous electrical nerve stimulation (TENS) and pulsed radiofrequency therapy are two examples of nerve-stimulation procedures that can alleviate pain by altering nerve signals. These methods involve using deficient levels of electricity or magnetic fields to stimulate healing and reduce discomfort.
Surgical Interventions for Severe Cases
Decompression Surgery: Relieving Nerve Pressure
Surgical decompression may be an option when conservative measures fail to alleviate symptoms of severe pudendal nerve entrapment. This surgical technique aims to relieve the entrapped nerve so it can function more normally. Neurolysis and neuroplasty are surgical procedures that relieve pressure on the pudendal nerve.
Neuromodulation: Managing Pain Signals
Implanted devices deliver electrical or magnetic stimulation of the afflicted nerves in neuromodulation procedures. Individuals who have not found relief from conventional treatments for pudendal nerve entrapment may find it helpful to try spinal cord stimulation or peripheral nerve stimulation to assist in modifying pain signals.
Nerve Grafting: Restoring Nerve Function
Nerve grafting may be an option in cases of significant injury or compression of the pudendal nerve. The injured section of the pudendal nerve is repaired or replaced during surgery using a nerve graft harvested from another area of the patient’s body. Restoration of nerve function and relief of symptoms are the goals of nerve grafting.
The Value of Integrating Different Treatment Methods
Multidisciplinary care is typically necessary for treating pudendal nerve entrapment. Comprehensive and tailored treatment plans can be provided through the combined efforts of healthcare professionals from various fields, including pain management specialists, physical therapists, psychologists, and surgeons. With this comprehensive strategy, patients have a higher chance of experiencing successful condition management and enhanced quality of life.
Lifestyle Modifications and Self-Care Strategies
Managing pudendal nerve entrapment requires a multifaceted approach, including medical treatment, behavioral changes, and self-care. Individuals’ symptoms, general health, and quality of life can all benefit from the regular use of these techniques. Some valuable approaches are listed below.
Ergonomic Adjustments for Sitting and Standing
The pressure on the pudendal nerve can be relieved by adopting more ergonomic sitting and standing positions. If you have to sit for prolonged amounts of time, try using a cushion or a specific seat pad with a cutout to lessen the strain on your pelvic area. Keep your back straight by sitting up straight, balancing your weight equally, and working at a workstation that allows you to stand up straight.
Pelvic Floor Relaxation Exercises: Strengthening and Relaxing Muscles
Pelvic floor relaxation techniques help reduce stress and enhance the performance of the pelvic floor muscles. The pelvic floor muscles are actively contracted and released throughout these routines.
Kegel exercises, like others, can strengthen the pelvic floor muscles and provide more structural support for the pelvic organs. Consult a pelvic floor physical therapist for guidance on appropriate exercises and techniques.
Stress Management Techniques: Finding Relief
Pudendal nerve entrapment symptoms might be made worse by stress. The detrimental effects of stress on the human body and mind can be mitigated by using stress management strategies.
Deep breathing techniques, meditation, yoga, or simply participating in relaxing hobbies and activities can help. Finding effective methods of relieving stress is crucial if you want to control your symptoms and boost your health.
Diet and Nutrition Tips for Reducing Inflammation
The inflammation and pain caused by pudendal nerve entrapment may be alleviated by adopting a healthy, anti-inflammatory diet. Consume many nutritious foods, such as fresh produce, whole grains, lean proteins, and healthy fats.
To reduce inflammation, reducing or eliminating your consumption of processed foods, sugary snacks, and foods high in saturated fats is best. The advice of a licensed dietician can be tailored to your nutritional requirements.
Prevention and Long-Term Management
Preventative interventions and long-term management tactics can help lower the likelihood of developing pudendal nerve entrapment and improve symptoms, which is not always possible. Preventative measures can improve health and lessen the severity of symptoms associated with pudendal nerve entrapment. Fundamental approaches include the following:
Preventive Measures for Reducing the Risk of Pudendal Nerve Entrapment
Not knowing what causes pudendal nerve entrapment can be frustrating, but there are strategies to lessen your chances. Preventing nerve irritation or compression may be possible by avoiding activities that place undue tension on the pelvic muscles or involve extended sitting on hard surfaces. Safe and correct procedures during childbirth and pelvic region surgery can also help decrease the likelihood of pudendal nerve entrapment.
Regular Exercise and Maintaining a Healthy Weight
Long-term therapy for pudendal nerve entrapment should include regular exercise and keeping a healthy weight. Regular low-impact exercises like swimming, walking, or yoga can benefit strength, flexibility, and blood flow.
These moves help keep your pelvis steady, ease muscle tension, and maintain healthy nerve function. Furthermore, a healthy weight might reduce nerve compression risk by easing the pelvic area strain.
Proper Posture and Body Mechanics: Essential Considerations
Correct posture and body mechanics are necessary for those suffering from pudendal nerve entrapment. The pelvic region is relieved of some pressure when the body is positioned correctly.
It’s best to sit up straight, with your back properly supported. Reducing nerve pressure is also facilitated by avoiding static positions such as prolonged sitting or standing. Avoiding unneeded stress on the pelvic region can be as simple as paying attention to body mechanics when performing everyday tasks like lifting heavy objects or bending.
Ongoing Self-Care Practices for Long-Term Symptom Management
Consistent self-care behaviors are crucial for symptom management and long-term health maintenance. This involves carrying on with stress management practices, healthy eating habits, and pelvic floor relaxation exercises.
Practicing relaxation techniques regularly, finding stress-relieving activities to partake in, and eating healthily can all aid in symptom management and preventing flare-ups. Ongoing symptom management and high quality of life can be achieved by maintaining regular contact with healthcare professionals, such as pelvic pain specialists or physical therapists, for regular examinations and adjustments to the treatment plan.
Individuals with pudendal nerve entrapment can take charge of their health and well-being using these preventative actions and long-term care options.
Book with us Today!
Pudendal Nerve Entrapment can significantly impact a person’s quality of life. Still, they can find relief and regain control with understanding, a proper diagnosis, and the right treatment.
Patients can empower themselves to long-term management by instituting lifestyle modifications, adopting coping strategies, and practicing preventive measures. Remember that seeking professional assistance and establishing a solid support network is crucial for a better tomorrow.
Are you prepared to manage the discomfort caused by pudendal nerve entrapment? Check out our website for helpful self-care tips and exercises. See us now to get started on the path to relief and a better way of life.
More About Pudendal Neuralgia & Pudendal Nerve Entrapment
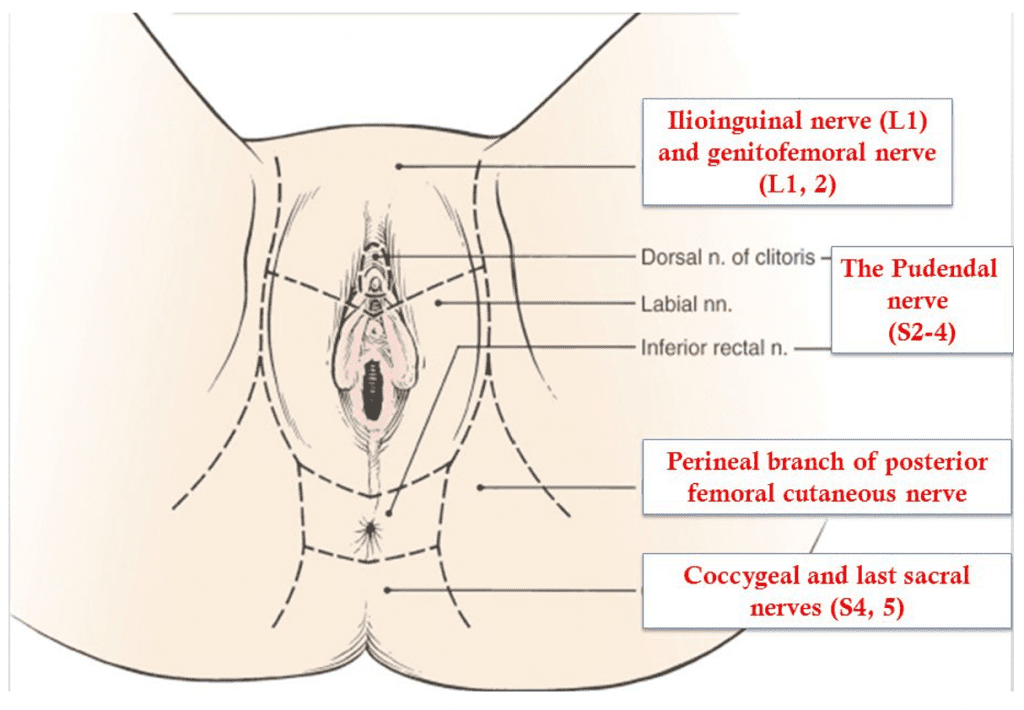
Innervation of the perineum
Pudendal nerve entrapment is almost always caused by some traumatic event to the pelvis. This may be pelvic surgery (with or without mesh), difficult childbirth, athletic injury, falls, and other accidents. A repetitive injury, such as bicycle seat pressure on the pelvic floor, may also lead to pudendal nerve entrapment (cyclist syndrome).
Diagnosis of pudendal nerve entrapment is not easy and relies heavily on taking a detailed history. Pain is located in the vagina, vulva, clitoris, perineum, and rectum, and it may involve one or all of those areas. Pain is more severe with sitting than with standing or lying down, and sitting on the toilet is generally better than sitting on a chair. Most of the patients with real nerve pain injuries have pain on one side only, or one side is significantly more painful than the other. Chronic Pelvic Pain is generally more severe with urination, bowel movements, and intercourse. Some patients may also have difficulty emptying their bladder (hesitancy) and bowel (constipation). One of the most debilitating symptoms of pudendal nerve entrapment is a sensation of continuous sexual arousal (persistent genital arousal disorder – PGAD). Patients often reduce this sensation by masturbation which only provides temporary relief.
A pioneer in the treatment of pudendal nerve entrapment and my mentor, Professor Roger Robert, has developed Nantes criteria which greatly assist in diagnosing this condition. Studies have shown that patients who more closely meet the criteria have better outcomes from the surgical decompression of the nerve.
Nantes Criteria
| Inclusion criteria |
|
|
|
|
|
| Exclusion criteria |
|
|
|
|
| Complementary criteria |
|
|
|
|
|
|
|
|
| Associated signs |
|
|
|
|
|
|
|
|
|
Inferior rectal nerve
Cutaneous branch of the obturator nerve
Lateral cutaneous branch of iliohypogastric nerve
Femoral branch of genitofemoral nerve
Posterior femoral cutaneous nerve
Lateral femoral cutaneous nerve
Iliohypogastric nerve
Clitoral/perineal nerves
Femoral nerve
Genital branch of genitofemoral nerve
Other nerves innervating the pelvis
Pain in pudendal nerve entrapment is of neuropathic nature, which means that patients feel burning tingling and numbing sensation (paresthesia). Some patients have the sensation of a foreign body located in the rectum or vagina (allotriesthesia) and may describe it as a “red hot poker” in the rectum. Some patients do not experience any chronic pain but have complete or partial numbness in the area of innervation of the pudendal nerve.
Additional tests such as magnetic resonance neurography (MRN), pudendal nerve motor terminal latency (PNMTL), another electrophysiologic testing, or sensory threshold testing are generally not accurate enough to diagnose pudendal nerve entrapment. A CT-guided pudendal nerve block is a part of Nantes criteria, and an important step in the diagnosis and treatment of pudendal nerve entrapment. Lack of relief of pain immediately after a CT-guided pudendal nerve block means that pain originates in another structure or is transmitted by a different nerve other than pudendal.
Conservative treatments of pudendal neuralgia consist of:
- Avoidance of additional injury – patients need to immediately stop the activities that lead to injury of the nerve in the first place. For example, if nerve pudendal neuralgia was caused by riding a bicycle, the patient has to immediately stop cycling. Of course, this cannot be done in cases where the patient developed pudendal neuralgia as a result of surgery or childbirth
- Protecting the nerve by using sitting cushions, zero gravity chairs, or kneeling chairs
- Medications including oral medications and vaginal/rectal suppositories
- Appropriate pelvic floor physical therapy (to minimize pelvic floor muscle spasm)
- Botulinum toxin A injections to pelvic floor muscles (to minimize pelvic floor muscle spasm)
- Pudendal nerve blocks using CT, ultrasound, or in some cases unguided transvaginal blocks
- Pudendal nerve injections with amniotic fluid and liquified amniotic membrane
- Ablation procedures – pulse radiofrequency ablation (pRFA) and cryoablation
- Nerve stimulators and spinal cord stimulators
- Surgical decompression of the nerve. Pudendal nerve decompression can be done using several different approaches: transgluteal, transischorectal, transperineal, and laparoscopic/robotic.
The transgluteal approach is an original technique described by Professor Roger Robert in Nantes, France, and very significantly modified by me. This approach offers by far the best access to the pudendal nerve, therefore allowing for the most complete decompression. One of the earlier drawbacks of the technique was cutting of the sacrotuberous ligament which in some cases could lead to pelvic instability. The risk of that instability was eliminated when I began repairing the sactotuberous ligament. Cutting of that ligament allows access to the nerve and frees it from the scar tissue or surgical materials, but after nerve decompression is accomplished sacrotuberous ligament should be repaired.
Other modifications that I have introduced to the pudendal neurolysis surgery were:
- Use of surgical microscope for better visualization of the nerve and surrounding structures
- Use of Nerve Integrity Monitoring System (NIMS monitor) to aid with identification of pudendal nerve. It is especially helpful in cases when the nerve is significantly scarred, and in cases of repeat surgery.
- Use of a pain pump that delivers a local anesthetic to the nerve for about seven days after surgery. This decreases pain levels and is thought to reverse central sensitization (memory of pain in the brain). This step may lead to faster recovery and resolution of pain after surgery.
- Nerve wrapping with an adhesion prevention barrier decreases the risk of scarring or re-scarring of the nerve after surgery. Several years ago, I switched from regular nerve wraps to wrapping the nerve with an amniotic membrane product. In addition to anti-adhesion (anti-scarring) properties, the amniotic membrane contains nerve growth factors that promote nerve healing. It also may have the ability to attract your own body’s stem cells close to the nerve, which further helps with nerve regeneration.
- Use of suction dressing after the closing of the skin to minimize the risk of wound infection
The microscope used for transgluteal pudendal surgery. On the left of the screen NIMS monitor used for monitoring the nerve during surgery
Laparoscopic/robotic procedure is less invasive, but it does not offer as good of access to Alcock’s canal as transgluteal procedure does. It may be effective in cases where the nerve compression is limited to the small area, but the location of compression may be difficult to determine prior to surgery.
In my practice, I perform both transgluteal and robotic nerve decompression procedures, but I believe that since the transgluteal technique offers better access and allows for decompression of the larger part of the pudendal nerve, it should be a preferred approach. Even though the recovery time is longer compared to the laparoscopic procedure, the benefits of more complete nerve decompression are very important when considering the choice of surgery.
Overall, the results of surgery show that the majority of patients have significantly decreased pain, and benefit from pudendal nerve decompression procedures.
If you or someone you know experiences pain with sitting in the clitoris, vulva, penis, scrotum, perineum, or rectum, call 480 599-9682 or email [email protected] to learn more about available treatments.
View of the pudendal nerve through the microscope (nerve in the blue rubber band – vessel loop)
What to expect before and after transgluteal nerve decompression surgery
1. Prior to surgery Dr. Hibner and his team will use some or all available non-invasive methods to help you with your pain. They may include physical therapy, suppositories, oral medications, nerve ablations, injections of amniotic fluid/membrane products.
2. Decision for the surgery is made together by the patient and Dr. Hibner. It is based on all the information from the patient’s history, exam, radiology results, any additional testing. Also, the fact that all offered conservative treatments have failed is taken into account when deciding on surgery.
3. Transgluteal pudendal nerve decompression is Dr. Hibner’s preferred way to free up the nerve from scar tissue but in certain cases robotic approach or highly selective approach to the pudendal nerve, branches may also be chosen.
4. Prior to the surgery please follow all the pre-operative instructions which will be given to you during the visit
5. For the transgluteal decompression surgery you will be positioned on your abdomen (prone) and the incision will go on the buttock on the operated side. It will measure anywhere from 2 to 4 inches.
6. When you wake up from surgery in the recovery area you will have a catheter in your bladder, a pain pump dripping local anesthetic on your nerve, and negative pressure dressing on the skin over the incision. You will receive a bag to wear over your shoulder for the pain pump and device providing suction to the dressing). It is very important to be gentle with the pump to avoid dislodging the catheter. If the pain pump catheter is dislodged, it cannot be replaced.
7. You should feel numbness in the area of the pudendal nerve (where the pain was before surgery) but the incision over the buttock will be quite tender. Pain pump medication does not reach the muscles or skin of the buttock, and it is only meant to provide pain relief in the nerve.
8. Most patients spend one night in the hospital. A very rare two-night stay is required
9. You should be active and try to walk with support the next day after surgery. This prevents a loss of muscle and could also decrease the risk of nerve scarring. Please be very careful when moving and walking not to pull the pain pump.
10. You will be discharged home with pain medications and instructions on how to use the pain pump and negative pressure dressing. You may need to return to the clinic for the dressing and pain pump removal, or we will instruct you how to do it yourself. When the pain pump comes out your pain may increase until the nerve begins healing.
11. You can shower 2 days after surgery. Try to avoid making the area of the incision wet. You can wrap that area with a large garbage bag for the time of surgery. Water is not going to contaminate the incision but may make the adhesive covering the pain pump catheter wet leading to the earlier removal of the pump.
11. Most patients can travel within 5-7 days after surgery but a longer stay is encouraged before traveling back home.
12. You can resume the activity after surgery but avoid doing things that significantly increase your pain. Sitting should be avoided. If surgery was done on one side only try to sit on the opposite buttock.
13. Do not flex your hip(s) over 90 degrees. This may lead to pulling apart the sacrotuberous ligament which was repaired during surgery. This ligament takes approximately 6 months to heal. You should therefore avoid squatting, taking two steps at a time when walking upstairs, etc.
14. You should resume pelvic floor physical therapy approximately 6 weeks from surgery. You will be given instructions for you and your physical therapist regarding recommended therapy.
15. It may take 3-4 months to start feeling the improvement in pain. It is normal to have better and worse days. When you have a better day please be careful not to overexert yourself. Follow the instructions of your pelvic floor physical therapist on physical activity.
16. Please continue to take all your medications until you are instructed to stop. You can continue vaginal/rectal suppositories, but you should be decreasing the number of narcotic pain medications you take.
17. Generally we do not schedule patients for in-person postoperative visits. Care can be done over the phone or by telemedicine.
18. Maximum healing may take 18 to 24 months from surgery. After 2 years from surgery majority of patients have less pain or no pain. If you continue to be in pain, we will look for other solutions to help you with your condition.
Outcomes
Outcomes of this procedure depend on the causes of nerve compression, the degree to which the nerve was compressed, and how much time elapsed between the injury and surgery. Unfortunately, the degree of nerve damage is difficult to assess before surgery. From my extensive experience of doing hundreds of pudendal decompression surgeries, approximately two-thirds (66%) of patients benefit from this procedure. This number includes all the patients, even those with severe nerve injury. That means that patients with less severe nerve injury may benefit from the procedure even more.

Patient positioned for Pudendal decompression surgery. The incision the buttock marked with a pen. Electrodes are placed for monitoring the pudendal nerve (NIMS monitor).
A little history…
Pudendal neuralgia has been recognized by medicine in the book published in Philadelphia in 1871 – “The Change of Life in Health and Disease”. The knowledge of pudendal neuralgia was almost lost until the late 1980s. French neurologist Dr. Gerard Amarenco reported on a series of patients with “syndrome du cyclist”, the cyclist syndrome which occurs when a pudendal nerve is compressed between narrow bicycle seat and medial surface of ischial tuberosity (sitz bone). The first procedure to surgically decompress the pudendal nerve through transperineal technique (incision around the anus) was described in 1992 by Egyptian surgeon Dr. Ahmed Shafik. Soon after my mentor Professor Roger Robert from Nantes, France described transgluteal pudendal neurolysis – decompression of the pudendal nerve with an approach through the buttock. Professor Robert is not only an outstanding neurosurgeon, but also an anatomist, and this unique combination allowed him to develop the whole new procedure for pudendal nerve decompression.
I graduated from my fellowship in gynecologic surgery at Mayo Clinic in 2003 and opened pelvic pain practice in Phoenix in 2004. I started seeing patients with pelvic pain whose condition could not be explained by any disease known to me. So, in early 2005 I googled the symptoms: perineal/vaginal bringing pain with sitting. Several medical articles showed up, but most of them had one common name as one of the authors: Roger Robert. I then send the letter to Nantes France to Professor Robert if I could come to visit him and learn from him. In the summer of 2005, I traveled to Nantes and worked with Professor Robert for almost 3 weeks assisting him on numerous surgeries and seeing many patients in the office with him. I also worked with wonderful Dr. Jean Jacques Labat, a neurologist who assisted Professor Robert with diagnosing and treating patients before surgery, and with amazing radiologist Dr. Thibault Riant who taught me how to perform CT-guided pudendal nerve blocks. When I returned to Phoenix, I started seeing more and more patients with pudendal neuralgia and pudendal nerve compression, and I performed my first transgluteal pudendal nerve decompression in the fall of 2005. It was in the patient who developed pudendal neuralgia after removal of Bartholin’s gland. She did well after surgery and soon many more patients have followed. From the very first surgery, I started modifying the original procedure developed by my great mentor, Professor Robert. The first modification was repairing of the transected sacrotuberous ligament. There was a concern that leaving this ligament not repaired may cause instability in the sacroiliac joint. So, from the very first patient, I would repair sacrotuberous ligament the same way that an orthopedic surgeon repairs a ligament in the knee. Next, I incorporated the use of a neurosurgical microscope into the procedure. This allowed for significantly improved precision. The next modification was the use of an On-Q pain pump placed next to the nerve towards the end of surgery to provide postoperative analgesia and decrease central sensitization (memory of pain in the brain). The third modification was the incorporation of NIMS (nerve integrity monitoring system) to allow to the identification of the nerve in the setting of significant scarring. The next modification was the use of nerve wrap to prevent the reoccurrence of adhesions. Initially, I was using a collagen nerve conduit but a few years ago I switched to an amniotic membrane which in addition to preventing adhesions also contains factors/chemicals promoting nerve healing. The last major modification was the method in which I cut the sacrotuberous ligament. Cutting it in a Z fashion allows me for better access to the nerve and facilitates the repair at the end of surgery. Up to today, I have done several hundred of those procedures, most likely more than any other provider with exception of my amazing mentor, Professor Roger Robert.

From the left: Dr. Jean-Jacques Labat, me, Professor Roger Robert and Dr. Thibault Riant
For more information visit:
https://www.glowm.com/section_view/heading/pudendal-neuralgia/item/691
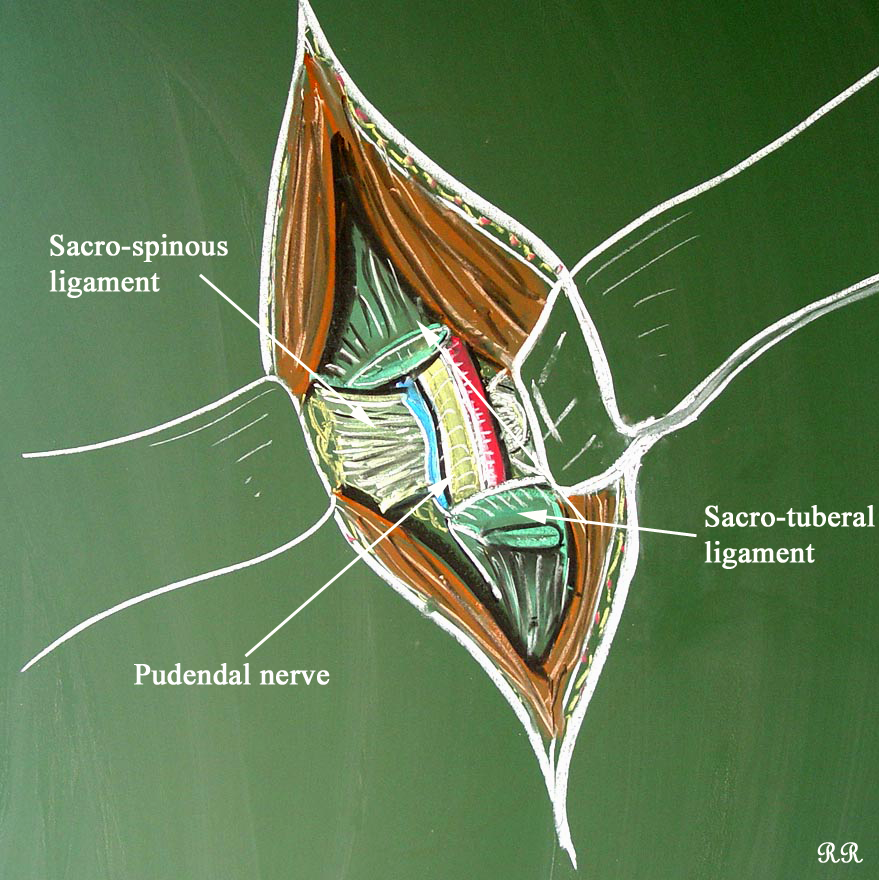
Drawing of the steps of transgluteal pudendal neurolysis by Professor Roger Robert
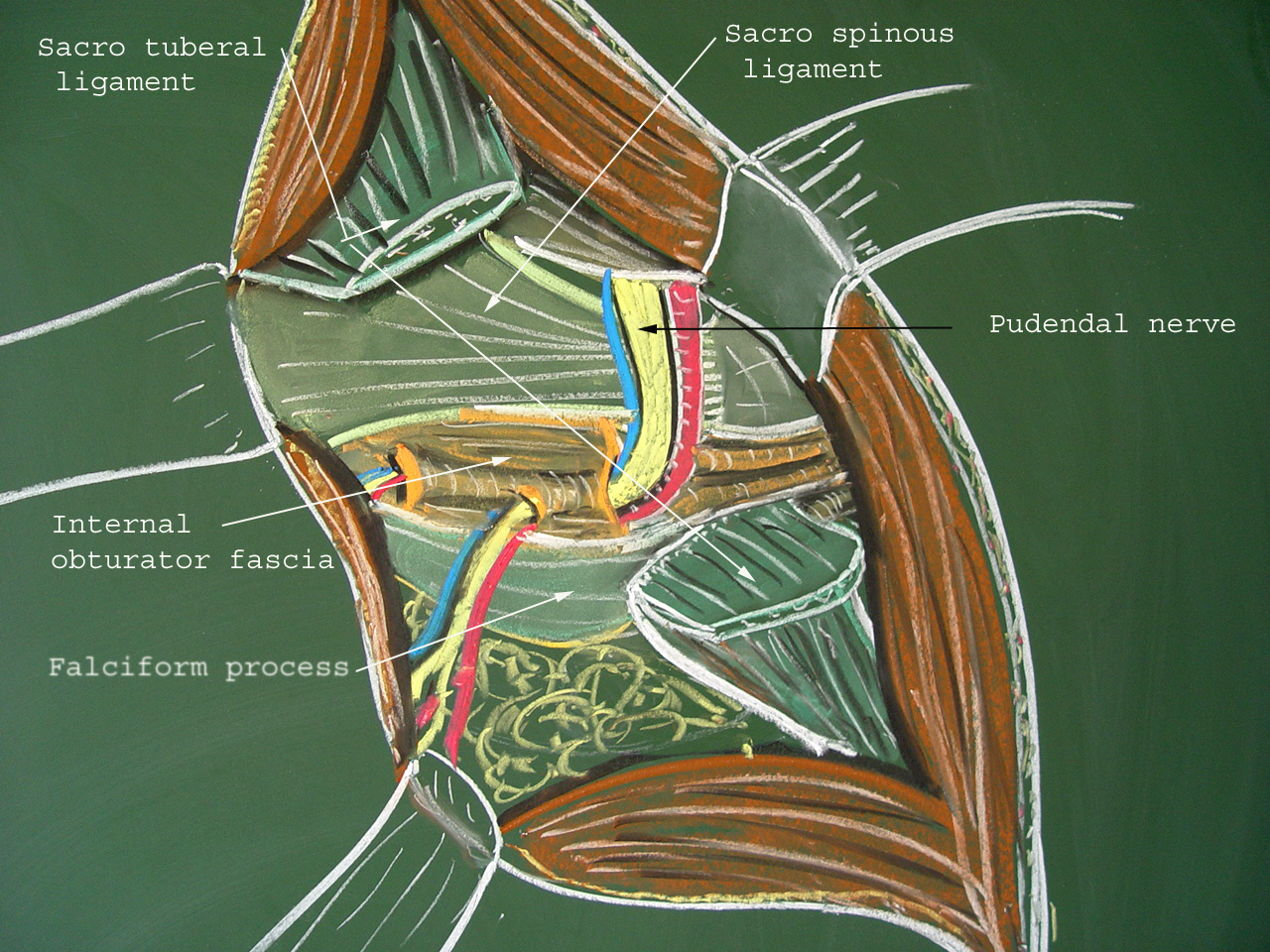
View of the opened space between the sacrotuberous and sacrospinous ligaments by Roger Robert
One of my numerous publications on pudendal neuralgia
Special thanks
Hard work and knowledge of many, many people went to the development of transgluteal pudendal decompression surgery the way I perform this procedure today. I would like to take this opportunity and thank Professor Roger Robert, Professor Oskar Aszman, Dr. Jamie Balducci, Dr. Jacek Bendek, Dr. Mario Castellanos, Dr. May Nour, Cindy Love, and many others. Big thank you from me and on behalf of my patients whom I was able to help with pain.
Pelvic Pain Frequently Asked Questions:
What is Pelvic Pain?
Pelvic pain in women is a common symptom that accounts for up to 30% of visits to a gynecologist, yet it is thought that close to 70% of cases of pelvic pain are not of a gynecological origin. Chronic pelvic pain is defined as pain that has been present for six months or longer, is localized to the pelvis, and is severe enough to cause functional disability requiring treatment. It is estimated that chronic pelvic pain affects 15% of women in the United States sometime during their lifetime. Yet, almost 60% of those patients do not have a proper diagnosis (and therefore no treatment). This is because this pain usually spans more than one specialty, and treatment requires physicians specifically trained in chronic pelvic pain. Those statistics are even more staggering because over 20% of women with pelvic pain miss work, close to 50% feel depressed, and in 90% of women, it affects their sexual life. Pain during or a complete inability to have intercourse significantly affects personal relations between the patient and her partner and further adds to suffering. Despite the fact that chronic pelvic pain in women is more common than coronary artery disease, asthma, or migraine headaches, very few physicians specialize in its treatment. Pain is often blamed on psychological issues, and patients are often referred to a mental health provider instead of getting treatment for their true, existing disease.
What conditions cause pelvic pain?
Multiple conditions may cause pelvic pain, often coexisting in one patient. Some of the more common conditions are:
- Endometriosis
- Interstitial cystitis/bladder pain syndrome
- Irritable bowel syndrome
- Spastic pelvic floor syndrome
- Adhesions in the pelvis and abdomen
- Pelvic congestion syndrome
- Pelvic nerve neuralgias
- Pain caused by pelvic mesh
The Arizona Center for Chronic Pelvic Pain offers comprehensive treatment for those and many other conditions causing pelvic pain.
What is pudendal neuralgia?
Pudendal neuralgia is a relatively unknown cause of severe pelvic pain.
In my practice, I define it as a pain located in the area of innervation of the pudendal nerve. Pudendal nerve entrapment is an impingement of the pudendal nerve caused by scar tissue, surgical materials, or mesh. Pudendal nerve entrapment is, therefore, one of the causes of pudendal neuralgia. However, other causes, such as inflammation, spasm of the surrounding muscles, or other nerve diseases, may also be reasons for pain.
What is pudendal neuralgia for men?
Pudendal neuralgia is defined as pain in the area of innervation of the pudendal nerve. In men, the areas affected can be the penis, scrotum, perineum, and rectum. Pudendal nerve entrapment is described as compression of the pudendal nerve from ligaments, scar tissue, or surgical materials, which leads to pudendal neuralgia. Some patients with pudendal nerve entrapment experience burning pain, but others may have a sensation of numbness. It may be present on one or both sides, and some patients experience problems with erection and pain with ejaculation. Penile numbness is one of the more frequent signs of pudendal neuralgia in men.
What are the symptoms of pudendal nerve entrapment?
How do you know if you have pelvic floor dysfunction?
Vaginal Spasms
Vaginal spasms, medically known as vaginismus, manifest as the involuntary contraction of the vaginal muscles, often leading to discomfort, vaginal pain, and difficulty or even an inability to engage in vaginal penetration, including sexual intercourse. This condition can be deeply distressing and can lead to a cycle of sexual pain and fear of further pain, complicating matters even further. Causes of vaginal spasms can range from physical conditions like vaginal dryness, often associated with vaginal atrophy, or conditions like vulvodynia, which results in chronic genital pain. In some instances, even routine medical procedures like a pap smear or a pelvic exam can become exceedingly painful due to muscle contractions. It’s also noteworthy that conditions such as pelvic inflammatory disease or a disturbance to the pudendal nerve, which caters to the pelvic area, might contribute to heightened sensitivity and muscle spasms.
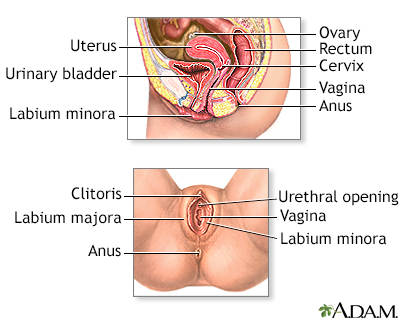
Treatment approaches for vaginal spasms are multifaceted and tailored to the root cause and individual’s symptoms. For those facing vaginal dryness or atrophy, particularly post-menopausal women, the application of vaginal estrogen can alleviate the associated discomfort, making the vaginal tissues more supple and less susceptible to pain. For others, vaginal dilators, often introduced under the guidance of a physical therapist, can gradually accustom the vaginal muscles to relax and accommodate penetration without reflexive contraction. Physical therapy, in fact, plays a pivotal role for many women as they learn techniques to gain more control over the pelvic muscles, reduce pain, and improve overall function in the pelvic area. While addressing the physical symptoms is essential, it’s also crucial to consider psychological or emotional factors that might contribute to or exacerbate vaginal spasms. Comprehensive care, combining medical intervention with psychological support, often provides the most effective relief for those navigating the challenges of painful intercourse and associated conditions.
Pelvic Floor Spasms
This condition is one of the “evil quadruplets” since it tends to co-exist with endometriosis, interstitial cystitis/bladder pain syndrome, and irritable bowel syndrome. The condition is like having a charley horse in the muscles that surround the vagina, urethra, and rectum. There are multiple reasons why this spasm happens.
Most often, it is some other pelvic pain condition that, through complex neural mechanisms, is irritating the pelvic muscle(s). Patients who have chronic pain from endometriosis, chronic pelvic pain syndrome, pelvic floor disorder, or pelvic trauma may develop spasms, which, unless treated, may last for many years. Some patients may also develop spasms after psychological trauma or even without any significant precipitating event.
Most commonly, patients with pelvic floor spasm(s) will experience pain during intercourse, urination, and bowel movement, as well as any physical activity. Generally, this pain persists from hours to days after sexual function or sexual intercourse. It may also persist after urination or bowel movement. Patients with muscle spasms may also have trouble starting the urine flow or difficulty in completely emptying the bladder. Because of that incomplete emptying, they often get up at night multiple times to urinate.
Pelvic floor spasm(s) may be easily identified during a physical exam or women’s health exam by a trained pelvic pain physician or pelvic floor physical therapist. Treatment consists of pelvic floor physical therapy and muscle relaxants.
The majority of patients are helped by those two modalities. In cases where muscle spasm is not relieved by pelvic floor physical therapy and muscle relaxants, botulinum toxin injections to the pelvic floor may be necessary. Treatment of the underlying pain is also very important.
In cases where pelvic floor muscle spasms developed because of other symptoms such as endometriosis, treatment of that underlying condition is very important. If someone has developed pelvic floor muscle spasm after placement of pelvic mesh, the mesh has to be addressed first before addressing muscle spasm.
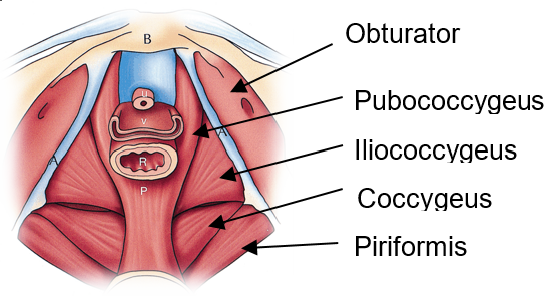
At Arizona Center for Chronic Pelvic Pain, we work with physical therapists in the Phoenix area and throughout the United States. We strongly believe that pelvic floor physical therapy is the most important part of relieving pelvic muscle spasm(s). In most cases, we will be able to recommend a physical therapist in your area or provide you with resources to find one. Strengthening weak pelvic floor muscles through pelvic floor exercises is critical.
Muscle relaxants are usually used in the form of a vaginal or rectal suppository and seem to be more effective than oral medications. Different formulations of suppositories exist, and they will be discussed with you during the visit. Botulinum toxin A (BotoxÒ) injections are offered to patients when physical therapy and suppositories fail. Those injections relieve muscle spasms and pain in the great majority of patients, but they may need to be repeated every few months. Because those injections are painful, they should always be done under sedation.
If you have difficulty finding a pelvic floor physical therapist in your area, please contact our office. We collaborate with therapists around the country, and we may be able to help you find one in your area. You can also visit the page of the International Pelvic Pain Society, the Women’s Section of the American Physical Therapy Association, or Herman and Wallace Pelvic Rehabilitation Institute to find a provider in your area.
If you or someone you know is experiencing pain related to pelvic floor muscle spasms, contact our office at 480 599-9682 or [email protected] to learn more about available treatments.
What to expect after BotoxÒ injection?
- BotoxÒ injections to pelvic floor muscles are almost always done in conjunction with pudendal nerve(s) block. The block is done to decrease pain after the procedure. When you wake up from the sedation after BotoxÒ injection, you will feel numbness in the pelvis, and you may have numbness in one or both of your legs. Numbness is completely normal and will disappear when the local anesthetic wears off.
- If you have numbness in your legs, you should avoid walking until the numbness goes away. You should have someone help you walk the first time you get up after the procedure.
- After the procedure, you may have difficulty emptying your bladder. Pelvic floor muscles are irritated immediately after the injection, and some patients may need a urinary catheter for a few days. Difficulty emptying the bladder goes away after BotoxÒ starts working and relaxes pelvic floor muscles.
- You may experience vaginal bleeding for 2-3 days after the procedure. It is completely normal, as long as the amount of bleeding is less than the menstrual period.
- After the local anesthetic wears off your pain may come back, and it may come back worse than it was before the procedure. This is because muscles are irritated from the injection. BotoxÒ starts working about one week after the procedure, but it may take 10-14 days to feel the relief of pain.
- It is very important to continue physical therapy after BotoxÒ Botulinum toxin by itself does not permanently cure muscle spasm, but it allows physical therapist to work more aggressively on your pelvic floor muscles.
- BotoxÒ wears off approximately 3-4 months after the injection. Some patients will not go back into spasm, but most will need a repeat injection. If you or your physical therapist feel your muscle spasm is returning, call our office to be scheduled for a repeat procedure.
Pelvic Floor Spasms
Pelvic floor dysfunction is a complex condition that encompasses a wide range of symptoms and abnormalities related to the pelvic floor. The pelvic floor, a supportive sling of muscles spanning the base of the pelvis, plays a pivotal role in the proper function of pelvic organs and the pelvic region. Dysfunction in this area can manifest in various ways, including hypertonic pelvic floor dysfunction, where the muscles of the pelvic floor remain persistently contracted, leading to pelvic muscle spasm or pelvic floor muscle spasm. This involuntary muscle tension can be distributed unevenly across the pelvic area, resulting in localized or generalized pelvic pain. Certain conditions like levator syndrome, caused by spasms in the levator ani muscle, and proctalgia fugax, an episodic, intense pain in the rectal area, are specific types of pelvic pain associated with pelvic floor muscle dysfunction. This hypertonicity can also negatively impact sexual function, with conditions like vaginismus, where the muscle spasm prevents or makes sexual intercourse painful. Moreover, disturbances in the pudendal nerve, which runs through the pelvic floor, can exacerbate or even initiate muscle spasms, thereby perpetuating chronic pain.
Many individuals suffering from pelvic floor disorders, including pelvic floor muscle spasms, experience challenges in their daily lives beyond pain. For instance, urinary incontinence and fecal incontinence, the involuntary loss of urine or stool, respectively, can result from abnormal muscle behavior or weakened connective tissue supporting the pelvic organs. Pelvic organ prolapse, where pelvic organs descend due to weakened support structures, is another consequence of pelvic floor disorder. Beyond these physical manifestations, the chronic pain and incontinence can significantly hinder one’s quality of life. Fortunately, therapeutic interventions such as pelvic floor physical therapy, overseen by a trained physical therapist, offer targeted exercises to strengthen, relax, and improve the coordination of the pelvic floor muscles. In more severe cases, muscle relaxants may be prescribed to alleviate persistent pelvic floor muscle spasms. Through a comprehensive approach addressing both the physical and emotional ramifications, individuals with pelvic floor dysfunction can find relief and reclaim control over their pelvic health.
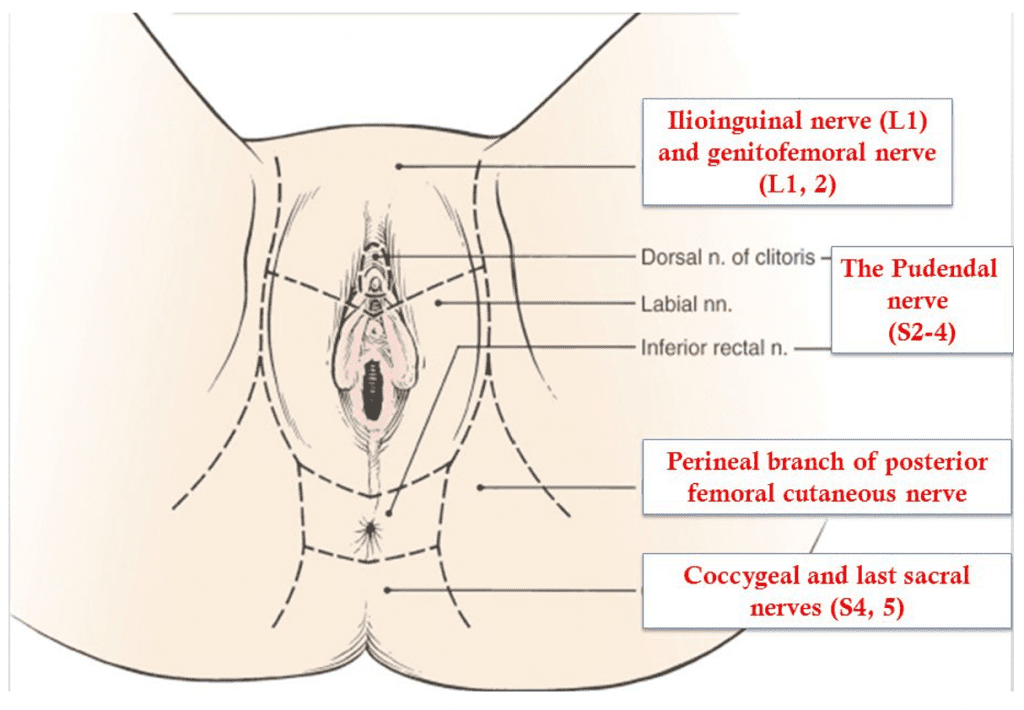
Pelvic floor spasms, a subset of the broader condition known as pelvic floor dysfunction, refer to the involuntary and persistent contraction of the muscles located in the pelvic region. The pelvic floor musculature, comprising a complex web of muscles, ligaments, and connective tissue, plays a pivotal role in supporting the bladder, rectum, and other pelvic organs. When these muscles undergo undue tension or muscle spasms, it can lead to a variety of uncomfortable and sometimes painful symptoms. Patients might experience challenges during sexual intercourse due to muscle tension, leading to compromised sexual health and function. Additionally, an overactive bladder, urinary incontinence, and even symptoms similar to irritable bowel syndrome can manifest when the pelvic floor muscles are in persistent spasm. As these muscles are closely associated with the ani muscle, any dysfunction in this region can severely impact daily activities and overall well-being.
Addressing Pelvic Floor Spasms
To address pelvic floor spasms, it’s vital first to identify the root cause of the dysfunction. For some, the muscle tension might be a reaction to conditions like pelvic organ prolapse, where the pelvic organs descend due to weakened support structures. For others, it might be a standalone issue. Once identified, tailored interventions can be suggested. Pelvic floor exercises, often guided by trained physical therapists, aim at both strengthening and relaxing the pelvic floor muscles. This ensures that they function optimally, providing the necessary support without being perpetually tense. Manual therapy can also be a beneficial intervention, where therapists use hands-on techniques to release muscle tension and alleviate spasms. In more severe cases, muscle relaxants might be prescribed to combat persistent pelvic floor muscle dysfunction. An integrated approach, focusing on both symptomatic relief and addressing the underlying cause, ensures that individuals can regain control over their pelvic health, ensuring a balanced and functional pelvic area.
Pain with sitting may be very debilitating since it often prevents patients from working (sitting at the desk) and participating in daily social activities (sitting to have a meal, travelling, going to the movies etc.) It may range from mild discomfort to severe pain preventing patient from sitting at all. Some patients find sitting on the doughnut cushion beneficial, others use zero gravity chairs or kneeling chairs and some patients do not set at all. They arranged their workspace using various types of standing desks.
Pain with sitting may be caused by the following conditions:
- pudendal nerve entrapment
- spastic pelvic floor syndrome
- pelvic congestion syndrome
If you or someone you know experience pain in the vaginal or rectal area related to sitting please call our office at 480-599-9682 or email [email protected] to learn about available treatments.
Most of the patients with pelvic pain feel better when they are standing unless it is a standing for prolonged time.
Pelvic pain typically related to standing is caused by pelvic congestion syndrome however patients with pudendal nerve entrapment may also have pain after prolonged standing.
Pelvic pain with standing may be related to hip or other joints or bones which are outside of scope of my practice.
If you or someone you know has pain with standing, call our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Pain with urination is a common symptom seen in many different conditions. Occasionally all of us experience it when we have a urinary tract infection. It becomes problematic when it is chronic and happens every time we go to the bathroom. It may range from mild discomfort to severe pain. It is very important to distinguish between pain when the bladder gets full, pain during urination, and pain at the end of urination.
Pain during and after urination is typically related to the spasm of the pelvic floor muscles. Pain in a full bladder is caused by interstitial cystitis/bladder pain syndrome.
Pain with intercourse is present in almost all patients with chronic pelvic pain.
It is the most common symptom for which patients visit our office. Understandably, a lack of intercourse may cause a loss of intimacy, often leading to significant anxiety, mental health issues, and emotional suffering. One of the most important parts of my job is helping people get their sexual health back and have pain-free intercourse.
Certain characteristics related to sexual activity allow for differentiation between the causes of pain with sexual intercourse:
Pain with sexual arousal, sexual pain, or foreplay may be caused by pudendal neuralgia or pelvic congestion.
Pain with entry or painful intercourse/painful sex may be caused by pelvic floor muscle spasm.
Pain with deep thrust may be caused by endometriosis or adhesions.
Pain with deep thrust in patients who had a hysterectomy may be caused by neuroma of vaginal cuff.
Pain with intercourse in the rear entry (“doggy”) position is common in patients with interstitial cystitis/bladder pain syndrome.
Pain after intercourse, sometimes lasting for a few days, is difficult in patients with pelvic floor muscle spasm or pelvic congestion.

Frequently Asked Questions:
What is dyspareunia?
Dyspareunia is a medical term for painful sexual intercourse.
Pain with Intercourse is also known as dyspareunia.
Causes of Pain with intercourse or dyspareunia can be a symptom of several conditions, such as:
-Vaginismus
-Vaginal dryness
-Infections (STDs, yeast, bacterial vaginosis)
-Uterine fibroids
-Endometriosis
-Pelvic inflammatory disease
-Cervical or vaginal cancer
-Interstitial cystitis
-Vulvodynia
What is vaginal atrophy?
Vaginal atrophy is a condition where the vaginal walls thin, become less elastic, and produce less lubrication, usually due to declining levels of estrogen during menopause. This can cause discomfort and pain with intercourse, urinary symptoms, and vaginal dryness.
What is vaginal dryness?
Vaginal dryness is a condition in which the vagina produces less natural lubrication, leading to discomfort and painful sexual intercourse. It can be caused by various factors such as menopause, hormonal changes, certain medications, and stress.
What is menopause?
Menopause is a biological process in which a woman’s ovaries stop producing eggs and her menstrual cycles end, typically occurring in the late 40s or early 50s. It marks the end of a woman’s reproductive years and the onset of various physical and hormonal changes.
What is a urinary tract infection?
A urinary tract infection (UTI) is an infection that occurs in any part of the urinary system (bladder, ureters, kidneys, and urethra) caused by bacteria. Symptoms can include frequent and painful urination, cloudy or strong-smelling urine, and lower abdominal pain. UTIs are common and can be treated with antibiotics.
Where are the pelvic floor muscles?
The pelvic floor muscles are a group of muscles that stretch like a hammock from the tailbone to the pubic bone and support the pelvic organs, including the bladder, uterus, and rectum. These muscles can be consciously controlled and play a role in bladder and bowel control, sexual function, and stability of the spine and hips.
What is sexual dysfunction?
Sexual dysfunction refers to a problem that occurs during any phase of the sexual response cycle and prevents an individual from experiencing satisfaction from sexual activity. This can include issues with desire, arousal, orgasm, or pain during intercourse. Sexual dysfunctions can be physical or psychological in nature and can impact an individual’s overall quality of life.
Is vaginal tissue the same as the endometrium?
No, vaginal tissue and endometrium are different tissues. The endometrium is the inner lining of the uterus that builds up and is shed each month as part of the menstrual cycle. The vaginal tissue is the tissue that lines the vagina and is more durable and less susceptible to changes than the endometrium. Endometriosis occurs when the endometrial tissue grows outside of the uterus, whereas vaginal tissue remains in its proper location.
What is endometriosis?
Endometriosis is a condition in which the tissue that normally grows inside the uterus (endometrium) grows outside of it, typically on the ovaries, fallopian tubes, and the tissue lining the pelvis. This tissue still responds to hormonal signals from the menstrual cycle and can cause pain, heavy periods, and infertility. It is a common gynecological condition, affecting about 1 in 10 women of reproductive age.
*Pelvic Surgery isn’t always necessary, and pelvic floor physical therapy may help with a medical condition concerning chronic pain in the pelvic muscle.
Pelvic pain with physical activity is usually caused by spasm of pelvic floor muscles. It may also be caused by abnormalities in hip joints and bones which is outside the scope of my practice.
If you or anyone you know experiences pelvic pain with physical activity, please contact our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Enduring the Monthly Misery of Menstrual Back Pain – Back Pain with Menstruation
Women understand the difficulty of enduring menstrual back pain every month. It is the type of pain that can turn even the most optimistic diva into a grumpy older woman.
But have no fear. We have your back (literally)! Many women experience menstrual back pain, which is more than a mere inconvenience. It can severely hinder your ability to perform daily tasks and enjoy your favorite pastimes.
This article will discuss the origins of this perplexing pain, the symptoms to watch out for, and some tried-and-true remedies to help you manage and prevent this monthly annoyance. Grab your heating pad and favorite snack, and let’s investigate menstrual back pain!

Causes of Back Pain During Menstruation
Women need to understand that there are a variety of factors that can contribute to back pain during menstruation. Understanding these causes can assist women in preventing and managing this pain. The following are common causes of menstrual back pain:
Muscle tension: When a woman is having her period, she will have uterine contractions, which cause tension in the muscles in the surrounding area, including those in the lower back. Because of this tension, one may experience discomfort as well as pain.
Poor posture: A change in posture is something that many women experience during their menstrual cycles. This change in posture can put additional strain on the muscles in the lower back. The pain in this area is exacerbated when you slouch or hunch over.
Heavy lifting: Because of increased fatigue and possible hormonal shifts, a woman may feel weaker than usual while menstruating. Lifting heavy objects can put a strain on the muscles in the lower back, which can lead to pain signals.
Endometriosis: This condition in which the uterine lining grows outside the uterus, causing suffering and uneasiness. Endometriosis can result in menstrual back pain.
Fibroids: These noncancerous uterine growths can cause painful cramps and back pain.
Ovarian cysts: These fluid-filled sacs can develop in the ovaries, causing lower back and abdominal pain and discomfort.
Menstrual back pain can have numerous causes. Give consideration to your body and seek medical attention if the pain is severe or continues for an extended period.
Tips for Reducing Back Pain with Menstruation
Back pain during menstruation can be debilitating, but there are measures you can take to alleviate the pain and enhance your quality of life. Here are some tips for dealing with menstrual back pain:
Use back support: Wearing a back brace or support can help relieve tension and pain in the lower back muscles. There are numerous back supports available at local pharmacies and online.
Exercise: Walking and yoga are gentle exercises that can help improve circulation and relax the lower back muscles. Consult your doctor before beginning a new exercise regimen.
Heat therapy: A heating pad or hot water bottle applied to the lower back can help relax tense muscles and alleviate pain.
Over-the-counter pain relief: Over-the-counter pain relievers like ibuprofen or acetaminophen can help alleviate menstrual back pain. Follow the prescribed dosage and consult your physician if you have any concerns.
Avoid heavy lifting: Heavy lifting can strain the lower back muscles, resulting in pain and discomfort. Try to avoid heavy lifting during your period, and if you must move something heavy, ask for assistance.
Maintain good posture: During menstruation, paying attention to your posture can prevent back pain. Try to sit and stand upright, avoiding slouching and hunching.
Relaxation techniques: Tension and stress can aggravate menstrual back pain. Try techniques such as deep breathing, meditation, or a warm bath to reduce stress and promote relaxation.
Remember, if you are experiencing severe or chronic back pain during menstruation, you must talk to your doctor. They can help you determine the underlying cause of the pain and provide additional treatment options.
Different Treatments for Back Pain During Menstruation
Although measures can be taken to prevent and manage back pain during menstruation, several treatment options are available for those experiencing more severe period pain. The following are common treatments for menstrual back pain:
Acupuncture: Acupuncture entails inserting thin needles into specified body points to stimulate nerve endings and alleviate pain. This treatment has been shown to reduce menstrual back pain effectively.
Massage therapy: Massage can alleviate menstrual back pain by reducing tension in the lower back muscles and improving circulation. Seek a licensed massage therapist with experience with women’s health concerns.
Spinal manipulation: This treatment involves applying pressure to the spine to alleviate pain and enhance function. Physical therapists and chiropractors can perform spinal manipulation to alleviate menstrual back pain.
Medications: As mentioned before, pain relievers like ibuprofen and acetaminophen that you can buy without a prescription can help with menstrual back pain. Your doctor may prescribe powerful pain medicines or muscle relaxants if the pain is severe.
Hormonal therapy: To alleviate menstrual back pain in women with endometriosis symptoms or fibroids, hormonal therapy may be recommended. Hormone replacement therapy can help regulate menstrual cycles and alleviate pain.
Surgery: In rare instances, surgery may be required to treat menstrual back pain-causing conditions such as endometriosis or ovarian cysts.
It is essential to discuss with your physician the optimal treatment options for your specific condition and level of pain. They can support you in identifying the root cause of your pain and developing a customized treatment plan to help you feel your best.
If you or someone you know experiences severe menstrual pain, don’t hesitate to get in touch with our office at 480-599-9682 or [email protected] for information about available treatments.
Conclusion
Back pain associated with menstruation can be a frustrating and unpleasant experience for many women. You can effectively manage pain and discomfort using painkillers, heat therapy, good posture, exercising, and getting sufficient rest.
In addition, those with severe menstrual back pain can access various treatment options, including acupuncture, massage therapy, and spinal manipulation. It is essential to discuss with your physician the optimal treatment options for your specific condition and level of pain.
You can reduce the impact of menstrual back pain on your daily life and feel your best throughout your menstrual cycle with the proper care and attention.
Pain with menstruation is typically caused by endometriosis or adenomyosis. It is important to remember that because of hormonal fluctuations, the pain threshold is lowered during that part of the menstrual cycle, and any pain may be perceived as more severe.
If you or someone you know experiences significant pain during menstruation, call our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Childbirth is one of the happiest moments in any woman’s life. Unfortunately, some patients may develop pelvic pain after delivery. In most cases this pain goes away within few weeks but in some it remains for much longer. There are multiple causes of pelvic pain after childbirth but most commonly it is of musculoskeletal origin. Some patients, especially after vaginal delivery, may develop spasm of pelvic floor muscles. This is more likely to happen in patients who had a big baby, had a procedure to help deliver the baby (vacuum or forceps) or had a big episiotomy or tear. In a small percentage of those patients, pain may be caused by nerve injury, specifically pudendal nerve or one of its branches. It is hard to initially distinguish between nerve and muscle injury because symptoms are similar, and diagnosis requires a physician who is familiar with pelvic floor disorders and nerve disorders to make that diagnosis.
Another type of pain which may occur after delivery is caused by pelvic varicosities which form during pregnancy. It is called pelvic congestion syndrome. It is characterized by heaviness sensation in the lower abdomen with prolonged sitting or standing with occasional sharp shooting pain. Many gynecologists do not recognize pelvic congestion as a condition which may lead to pelvic pain and that is why it is so important to see a provider who specializes in pelvic pain and can offer treatments for pelvic congestion.
If you or someone you know is experiencing pain after vaginal childbirth, please contact our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Pain with ovulation is called mittelschmerz. It is experienced by about 20% of women in some or all cycles. It occurs roughly halfway between menstrual cycles. It is usually sharp seven and located in the lower abdomen either on the left or right side. It is unknown why this condition happens and usually treated with nonsteroidal anti-inflammatory medications.
Pain with ovulation may also happen in patients who have pelvic adhesions which occurred as a result of previous surgery, endometriosis, infections or trauma. When ovary is trapped in the scar tissue it is not able to freely release an egg and causes pain. This pain may be relieved by surgically removing the adhesions.
If you or someone you know experiences pain with ovulation after surgery, infection, trauma or in the setting of endometriosis please call 480 599-9682 or email [email protected] to learn about available treatments.
Motor vehicle accident or any other accident is very traumatic and painful event. It is even more traumatizing when pain remains after healing ends. Some patients may develop persistent pelvic pain after a traumatic event even if there was no direct trauma to the pelvis. Patients who develop pain after accident often develop spasm of the pelvic floor muscles. Without direct trauma this spasm develops when patients are bracing for impact. Pelvic floor muscle spasm may be appreciated on the pelvic exam by a provider knowledgeable in this condition. Alternatively, patients with pelvic pain after accident may also suffer from compression or injury of one of the pelvic nerves. If pain is located in the vulva, vagina, penis, scrotum, perineum or rectum it may be caused by injury to the pudendal nerve. If that pain is in the lower abdominal or groin it may be caused by injury to ilioinguinal or genitofemoral nerve.
If you or someone you know experience pelvic pain after traumatic accident, please contact our office at 480-599-9682 or email [email protected] for more information on available treatments.
Patients undergo surgery with hope of treating the existing problem, so when the pain develops after the procedure, it is very disheartening even if the original problem was successfully addressed. This is even more complicated when patient had surgery to help with existing pain and ends up with the pain that is more severe than the pain she went in.
Pain after surgery depends on the type of surgery, positioning for the procedure and type of surgical materials used.
Type of surgery – pelvic surgery may lead to pelvic floor muscle spasm. Back surgery may lead to back muscle spasm which may lead to pelvic floor muscle spasm. Any open abdominal or pelvic surgery may lead to adhesions which may cause pelvic pain. Minimally invasive procedures such as laparoscopy or robotic surgery decrease the risk of adhesion formation after surgery. Any incision in the abdomen whether open or minimally invasive has a small risk of injuring abdominal wall nerves such as ilioinguinal or iliohypogastric.
Positioning for surgery may cause compression of certain pelvic nerves which in turn may lead to pain. Nerve blocks and nerve ablations may help in cases of nerve pain related to positioning.
Surgical materials – relates to the use of permanent vs. dissolvable sutures and pelvic mesh. In surgery both permanent and dissolvable sutures are used however, the latter are used much more often. Sometimes permanent sutures may have higher risk of causing inflammation and pain. For that reason, review of operative reports of previous surgeries is particularly important. Pelvic mesh is known in some cases to cause pelvic pain. In patients who have developed pain after surgery involving use of polypropylene mesh the possibility of mesh causing pain should be considered very seriously.
If your pain started as a result of surgical procedure it is very important that you provide us with the operative report and pathology report (if any) of this procedure. It is best if they are uploaded early so they can be reviewed prior to your visit. On instructions how to upload your documents please see section “New Patients”
If you or someone you know developed pain after pelvic surgery, call our office at 480-599-9682 or email [email protected] to learn more about available treatments.
Psychological traumatic event may be devastating to any patient at the time when it happens, but a lot of patients develop lasting effects of such a trauma. They are seen in women and men who are survivors of sexual violence, domestic violence, who have lived through sickness or death of a close relative or friend and many other traumatizing situations. It may happen in people who have highly stressful jobs or who have survived an accident, even without any trauma to the pelvis. In children it may happen during the divorce of their parents.
Many patients develop pelvic floor muscle spasm after psychological trauma and is seen both in women and men. It is a mechanism seen in some animals who tuck their tails under in response to stress or trauma and is caused by the spasm of the pelvic floor muscles. Many highly effective treatments are available for pelvic floor muscle spasm ranging from medications, to physical therapy and injections.
If you or someone you know is experiencing pelvic pain related to psychological trauma, please call our office at 480-599-9682 to learn more about available treatments.
It is estimated that up to 90% of women experience pain with onset of menstrual periods (menarche). It is called primary dysmenorrhea and by itself it does not mean any specific disease. With time and use of non-steroidal anti-inflammatory (NSAID’s) medications or oral contraceptives as well as healthy lifestyle, menstrual period pain in most of the patients improves. If this pain continues for 12 months after menarche, then it is called secondary dysmenorrhea. This ongoing pain with increases the chance of a specific condition causing pain. It is estimated that approximately 70% of patients with secondary dysmenorrhea have endometriosis. Diagnosis of endometriosis can only be done by the surgical procedure (laparoscopy, robotic procedure) and it cannot be reached by any other test. Physician may have a high suspicion of endometriosis but unless it is surgically proven, it is only a suspicion. It is especially important that this surgery is done by a provider who is familiar with diagnosis, treatment endometriosis and minimally invasive surgery.
If you or someone you know is experiencing pain which started at first menstrual period, please call our office at 480-599-9682 or email [email protected] for more information about available treatments.
No Pain
Uterine fibroids, medically called leiomyoma, are benign tumors of the uterus. They may range in size from microscopic to as large as the size of basketball or bigger. Approximately 20 to 25% of women in reproductive age are affected by fibroids, and this incidence may go up to 40% in women who are older than 40. Patients who had their first menstrual period at the younger age, or with later than normal menopause, are at higher risk for fibroids. Fibroid tumors are the most common in African American women, and least common in women of Asian descent. They are also more common in women who have a first degree relative with fibroids.
The most common symptoms fibroids is abnormal, sometimes very heavy vaginal bleeding, heaviness, pelvic pressure. Occasionally patients may also experience the frequency of urination. Fibroids rarely cause pain but often lead to discomfort during intercourse or physical activity.
Fibroids can be diagnosed on gynecological exam but the size and location is usually confirmed with an ultrasound or MRI.
Treatment of fibroids may be medical, using interventional radiology techniques, or surgical. If fibroids are found during routine exam and they do not cause any symptoms one of the choices would be to do nothing and wait to see if fibroids increase in size or become symptomatic. It is important to remember that fibroids increase in size before menopause so delaying treatment for too long may make it more difficult. Uterine fibroids very rarely become malignant, so presence of fibroids without symptoms is not an indication for surgery. Medical treatments are designed to decrease the level of estrogens and to trigger the fibroids to shrink. It is done by using anti-estrogen oral medications or injections. Patients undergoing those treatments may experience significant menopausal side effects from low estrogen levels. Also, within few months of stopping this treatment, fibroids may regain their original size. Hormonal treatment is therefore rarely a permanent fix. Fibroids may also be treated with interventional radiology by plugging the vessels which feed blood to the fibroid. This treatment is quite painful and may have a risk of compromising blood supply to the whole uterus or other internal organs. Embolization of fibroids may also increase the risk to future pregnancy.
Surgical procedures include minimally invasive myomectomy or minimally invasive hysterectomy. Myomectomy is a procedure in which fibroids are separated from the uterus and remaining uterus is reconstructed to allow for future pregnancy. It can be performed using surgical robot even with the large size fibroids therefore avoiding large abdominal incision. Some patients who completed the childbearing may choose to have a minimally invasive hysterectomy. It potentially allows for faster recovery and return to work then in patients undergoing myomectomy. Also, because fibroids tent to reoccur, hysterectomy decreases the risk of future pelvic surgery.
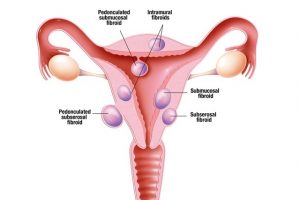
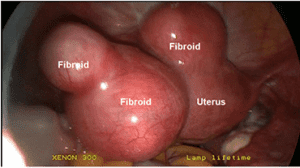
If you or anyone you know has symptomatic uterine fibroids, contact our office at 480 599-9682 or email [email protected] to learn about available treatments.
Ovarian Cysts: Causes, Symptoms, and Treatment Options
Ovarian cysts are a common gynecological condition that can affect women of all ages, particularly those of reproductive age. While many cysts develop as a normal part of the menstrual cycle and go unnoticed, others can cause discomfort, hormonal imbalances, or complications that require medical attention.
Understanding ovarian cysts’ different types, symptoms, and treatment options is crucial for maintaining reproductive health.
In most cases, cysts found in the ovaries are benign and resolve independently. However, medical intervention may be necessary when they persist, grow larger, or cause significant symptoms. Fortunately, advances in minimally invasive surgery, such as laparoscopy and robotic-assisted laparoscopy, have revolutionized the management of cysts, ensuring better outcomes with minimal disruption to ovarian function.
This article will explore the causes, symptoms, and treatment options for ovarian cysts, including special considerations for endometriosis-related cysts (endometriomas). If you or someone you know experiences recurrent cysts or concerning symptoms, seeking expert care can significantly improve long-term reproductive health and overall well-being.
What Are Ovarian Cysts?
Ovarian cysts are fluid-filled sacs that develop on or within the ovaries. They are common in women of reproductive age and often form a natural part of ovulation during the menstrual cycle. In many cases, cysts are harmless and resolve independently without causing noticeable symptoms.
However, certain cysts may grow larger, persist, or lead to complications requiring medical evaluation and treatment.
Ovarian cysts are fluid-filled sacs that develop on or within the ovaries and are common among women of different age groups. Studies indicate that approximately 7% of women worldwide will develop an ovarian cyst at some point in their lives.
In postmenopausal women, the incidence of ovarian cysts is about 18% over a 15-year period in the United States, while a European study reported a 21.2% incidence among healthy postmenopausal women. In children and adolescents, ovarian cysts are the most common tumors in infants and fetuses, with a prevalence exceeding 30%.
Among girls aged 5 to 18, 13.1% were found to have ovarian cysts measuring at least 1 cm in diameter, with a frequency of 1.8% in children aged 5-9 and 18.8% in those aged 10-18.
Causes and Types of Ovarian Cysts
Ovarian cysts can develop due to various factors, with the most common being functional cysts, which occur as part of the menstrual cycle. These include:
- Follicular Cysts: Form when a follicle (the sac containing an egg) does not release the egg as expected and continues to grow.
- Corpus Luteum Cysts: Develop after ovulation if the follicle fails to break down after releasing the egg, leading to fluid accumulation inside the follicle.
Other types of ovarian cysts include:
- Dermoid Cysts: Non-cancerous growths containing various tissues, such as hair, skin, or teeth.
- Cystadenomas: Fluid-filled cysts that form on the ovarian surface and may grow large.
- Endometriomas: Cysts associated with endometriosis, also known as “chocolate cysts,” which contain dark, thickened blood.
Symptoms of Ovarian Cysts
Many cysts found in the ovaries remain asymptomatic and are only discovered during routine pelvic exams or imaging studies. However, when symptoms occur, they may include:
- Sharp or dull pain in the lower abdomen or pelvis
- Bloating or a sense of fullness in the abdomen
- Irregular menstrual cycles or abnormal bleeding
- Painful intercourse
- Frequent urination or bowel movement discomfort due to pressure on surrounding organs
- Sudden, severe pelvic pain accompanied by nausea or vomiting, which may indicate ovarian torsion or rupture (a medical emergency)
When Is Treatment Necessary?
Most functional ovarian cysts resolve independently within a few menstrual cycles without requiring medical intervention. However, treatment may be necessary if a cyst:
- Persists for an extended period
- Grows larger than 5 cm
- Causes severe pain or other disruptive symptoms
- Has concerning features that suggest malignancy
- Becomes twisted (ovarian torsion) or ruptures, leading to internal bleeding
Minimally Invasive Surgical Treatment
When surgical removal is required, minimally invasive techniques such as laparoscopy These advanced techniques allow for:
- Greater precision in removing the cyst while preserving healthy ovarian tissue
- Reduced surgical trauma, leading to faster recovery times
- Minimal scarring and lower risk of postoperative complications
- Preservation of ovarian function, which is crucial for fertility and hormonal balance
Endometriomas: Special Considerations for Endometriosis-Related Cysts
Women with endometriosis may develop endometriomas, which are ovarian cysts formed when endometrial-like tissue grows within the ovaries. These cysts can negatively impact ovarian function, cause severe pain, and affect fertility. Unlike functional cysts, endometriomas do not resolve independently and often require surgical removal.
However, the removal of endometriomas should be performed by experienced surgeons to minimize the risk of damaging healthy ovarian tissue. Improper surgical techniques can reduce ovarian reserve (the number of remaining eggs), making it essential to seek care from a specialist trained in fertility-preserving surgery.
Seeking Expert Care for Recurrent Ovarian Cysts
If you or someone you know suffers from recurrent cysts, it is important to seek medical evaluation to determine the best course of action. Treatment options vary depending on the cyst’s type, size, and symptoms, and early intervention can help prevent complications.
Read more on conditions for women we treat, and reclaim your life today!
Schedule a Consultation Today
Our team, led by acclaimed Dr. Michael Hibner, specializes in the diagnosis and treatment of ovarian cysts. We focus on personalized, minimally invasive care to preserve fertility and hormonal function. Contact our office at 480-599-9682 or email [email protected] to learn more about available treatment options and schedule a consultation.
Müllerian Duct Anomaly
What Are Mullerian Anomalies?
Mullerian anomalies can affect up to four percent of the female population. The anomaly is considered a ‘hereditary disorder’; this indicates that this complication occurs during fetal development and is present during childbirth. As an embryo forms, the two paired Mullerian ducts will develop into the female genital tract, including the fallopian tube, uterus, cervix, and upper two-thirds of the vagina.
A Mullerian duct anomaly with congenital rectovaginal fistula is a very rare Mullerian abnormality or infection that may generate a gynecological and obstetric infection or complication, such as Dis colon rectum or problem with the rectum, colorectal dis, Crohn’s disease, colovesical fistula, diverticulitis, stool abnormalities, enterovesical fistula, fecal incontinence, inflammatory bowel disease, diverticular disease, which requires a surgery to treat or surgical intervention.
Mullerian abnormality, like rectovaginal fistula, is often associated with renal and axial skeletal abnormalities. Congenital rectovaginal fistula, imperforate anus (malformation of the anal canal which happens during childbirth), hypospadias (childbirth defect in boys), and other anatomical variants of cloacal dysgenesis can also be part of maldevelopment of the Mullerian and mesonephric duct derivatives.
For women, internal reproductive organs such as fallopian tubes, uterus, and upper part of the vagina derive from Mullerian ducts. Mullerian ducts are structures present in the fetus. Those ducts during fetal development undergo multiple changes, including fusion of the left and right sides.
Abnormalities in the formation of the Mullerian ducts lead to anomalies such as the bicornuate uterus, vaginal septum, or vaginal agenesis. Patients born with vaginal agenesis, also called Mayer–Rokitansky–Küster–Hauser syndrome (MRKH), do not have a uterus, cervix, or most of the vagina. Generally, the syndrome is discovered around the time of menarche because patients, despite normal sexual development, do not have a menstrual period.
Surgical treatments are available to create a functional vagina. One of the most successful procedures in patients with MRKH syndrome is the minimally invasive Vecchietti procedure. A fully functional vagina comparable to a normal vagina can be reconstructed using this procedure. It requires only three small laparoscopic incisions, which are cosmetically very desirable for a young patient.
Mullerian Defect On Female Reproductive Tract (Rectovaginal Fistula)
Just like the bladder, rectum, rectovaginal septum, and other organs in the body, a woman’s reproductive organs take form when she is still a fetus inside her mother’s uterus. These reproductive organs include the uterus and fallopian tubes, which develop from two ducts known as the müllerian ducts.
During normal development, these two ducts come together. However, there are times when fistula formation occurs. Fistula formation happens when the uterus and fallopian tubes don’t form as they should. These malformations are called Mullerian anomalies that make it difficult or impossible for a woman to get pregnant without getting surgery to treat it.
How Is The Condition Diagnosed?
Mullerian anomalies are commonly identified at the onset of puberty, when an adolescent begins to menstruate or when a young woman fails to get her menstrual period. Rectovaginal fistula may also be diagnosed when a woman experience trouble conceiving or maintaining a pregnancy. Some anomalies are associated with a common cause or symptom. Some of the symptoms that you might feel if you have a rectovaginal fistula are:
- Abdominal or pelvic pain
- Discomfort during sex
- Menstrual abnormalities
- Palpitation
- Stool abnormalities
Mullerian anomaly or infection and a reproductive underlying disease or condition can be diagnosed with imaging technology. Diagnostic testing may include:
- Pelvic ultrasound
- Three-dimensional ultrasound
- Magnetic resonance imaging (MRI)
- Hysterosalpingogram (HSG)
- Laparoscopy hysteroscopy
In most cases, Mullerian anomaly fistulae or fistulae such as vesicovaginal fistula and rectovaginal fistula can be left untreated, particularly when it does not significantly affect reproduction. Mullerian anomalies that prevent menstruation or cause significant pain in the urinary bladder, rectum, anus, and sigmoid colon usually requires surgical treatment or surgical repair. Surgery treatment depends on the extent of the individual fistula or if there is an existing underlying disease.
Can A Female With Mullerian Anomaly (Rectovaginal Fistula) Eventually Become Pregnant And Carry To Term?
Mullerian anomalies fistulae or fistula, specifically rectovaginal fistula, may affect fertility. But, if a woman undergoes treatment, the septated uterus can be corrected, which means getting rectovaginal fistula treatment or surgery (e.g., transvaginal repair) can improve the chances of having a successful pregnancy.
Women with a congenital reproductive anomaly, specifically rectovaginal fistula, who have not been able to complete pregnancy within six months of trying should visit a fertility specialist to get an examination or diagnosis of the fistula tract and surgery treatment. Arizona Center for Chronic Pelvic Pain (AZCCPP) has a fertility specialist with a magnificent reproductive surgical technique.
Surgery can repair the defect and eliminate discomfort in the rectum, anus, and bladder during menses or sexual relations, improving fertility and pregnancy outcomes. Arizona Center for Chronic Pelvic Pain’s (AZCCPP) reproductive surgeons is experienced in caring for adolescents and women with Mullerian anomalies. Our physicians are experts in performing surgery for rectovaginal fistula treatment.
ManagingPatients With Mullerian Anomalies
Managing patients with Mullerian anomalies doesn’t only focus on surgery or rectum and rectovaginal fist repair, such as anastomosis. Rather it also includes psychosocial counseling and a diagnosis of the symptoms of the fistula.
Psychosocial Counseling And Support
All patients with Mullerian anomalies should be offered counseling and encouraged to go and connect with peer support groups. Mullerian anomalies don’t only affect the patient’s bladder or rectum or make them abnormal. Fistulae, such as rectovaginal fistula, also have a psychological effect.
Most patients with rectovaginal fistula don’t only experience an abscess. Patients may also experience anxiety and depression that surgery can’t treat. They might even question their female identity and grieve their infertility. The symptoms of a fistula are not easy. Sometimes, surgery is not enough for a patient with a fistula to get better.
The best predictor of good emotional outcomes after their fistula diagnosis is a good relationship between the patient and their loved ones and the ability to share sentiments with family and friends.
Fertility
Patients with an abscess or fistula should be addressed with their future options for having children. An abscess or fistula can’t stop anyone who wants to be a parent. Adoption and gestational surrogacy are some of the patients with abscesses or fistula options to have children.
Assisted reproductive techniques with the help of a gestational carrier (surrogate) are thriving for women with fistula. Understanding the future fertility options of patients with fistula allows them to understand their potential for becoming parents, which may help them cope with the diagnosis, implications, and surgery.
Assessing The Patient’s Readiness
Nonsurgical or surgical treatment on the rectum, vagina, or other organs should wait until the patient is physically and emotionally ready to proceed with treatment. There are multiple risks of failure of nonsurgical or surgical treatment (e.g., interpersonal conflict, parental misunderstanding of diagnosis, poor motivation, unstable relationships, sociocultural factors, and mental health issues).
Cognitive issues that affect treatment adherence may include the following:
- Limited comprehension of the diagnosis and anatomy
- Young age
- Underlying learning disability
- Inadequate knowledge of the treatment process
- Lack of privacy and limited ability to travel to a clinic for close follow-up
Vaginal Elongation
Primary vaginal elongation repair by dilation is the appropriate first-line technique in most patients because it is safer, cost-effective, and patient-controlled than surgery. Primary vaginal elongation repair is a successful technique. When well-counseled and emotionally prepared, primary vaginal elongation repair lets 90 to 96% of the patients will be able to achieve anatomic and functional success.
General Gynecologic Care
Routine gynecology questions, which include asking for a patient’s personal information, are necessary, such as asking the date of the last menstrual period. The patient should also be asked about any vaginal bleeding, discharge, pelvic pain, abnormalities with their stool, pain in their rectum, as well as irritation with their skin.
What Types of Müllerian Anomalies Exist?
There are several different forms of müllerian anomalies ranging from the absence of a uterus to the formation of a half uterus or a double uterus to a uterus divided by a septum. All types affect the reproductive tract to varying degrees. They include:
Agenesis & hypoplasia: Mayer-Rokitansky-Kuster-Hauser syndrome is the most common. All or part of the müllerian tract fails to form or is extremely underdeveloped.
Unicornuate uterus (UU): When one müllerian duct is underdeveloped or fails to develop, a banana-shaped half-uterus is formed. A missing kidney or other kidney problems accompany this asymmetric anomaly more than they do other müllerian anomalies. This is a rare condition. Uterus didelphys (UD): Commonly referred to as a ‘double uterus.’ There may be complete duplication of the vagina, cervix, and uterus, and the two halves may be divided by a ligament of connective tissue. UD has the best pregnancy outcomes of all the MAs. Bicornuate uterus (BU): This is the most common form of müllerian anomaly. Described as a womb with two horns. The womb is not pear-shaped; instead, it is shaped like a heart, with a deep indentation at the top. This means that the baby has less space to grow than in a normally shaped womb.
Septate uterus: Occurs when the inside of the uterus is divided by a wall or the septum. The septum may extend only part way into the uterus or it may reach as far as the cervix.
DES-related uterus: A T-shaped uterine cavity, dilated horns, and malformed cervix and upper vagina may characterize this anomaly. A T-shaped uterus is sometimes caused by maternal ingestion of DES, although sometimes the cause is unknown.
Arcuate uterus (AU): The fundus of the uterus may be indented slightly both inside and outside. The shape is so slight that it is considered a variation of normal.
What is the most common uterine anomaly?
Bicornuate uterus (BU): This is the most common form of müllerian anomaly.
What causes uterus abnormalities?
A Uterine Abnormality may be a congenital uterine anomaly or may arise due to an infection or prior surgery.
Some of the most commonly seen congenital uterine anomalies are:
- Unicornuate uterus
- Bicornuate uterus
- Septate uterus
- Arcuate uterus
- Uterus didelphys
Correct Diagnosis
The most important steps in effectively treating Mullerian anomalies are a correct diagnosis of the underlying condition, correct evaluation for associated congenital anomalies, and psychosocial counseling. The treatment for Mullerian anomalies doesn’t only focus on treating the patient’s organs, such as the bladder, rectum, anus, etc. Counseling is also very important in addition to treatment or intervention to address the functional effects of genital anomalies.
Expert Care At Arizona Center for Chronic Pelvic Pain (AZCCPP)
We have top-rated pediatric and adolescent gynecologists (for children up to age 18) who are the best ones in Arizona and specialize in diagnosing and treating the most complex Mullerian anomalies in children and adolescent females and males, whether they’re pregnancy-related or otherwise.
We also have skilled reproductive endocrinologists (for adults over age 18) who have expertise in Mullerian anomalies in adults. At AZCCPP, we understand the importance of having a support system when it comes to considering treatment choices for Mullerian anomalies. The start of puberty and family planning are important times, and our team of experts is always here to speak to all of our patients about their options and what they can expect from our treatment plans.
If you or anyone you know has Mayer–Rokitansky–Küster–Hauser syndrome (MRKH) contact our office at 480 599-9682 or email [email protected] to learn about available treatments.
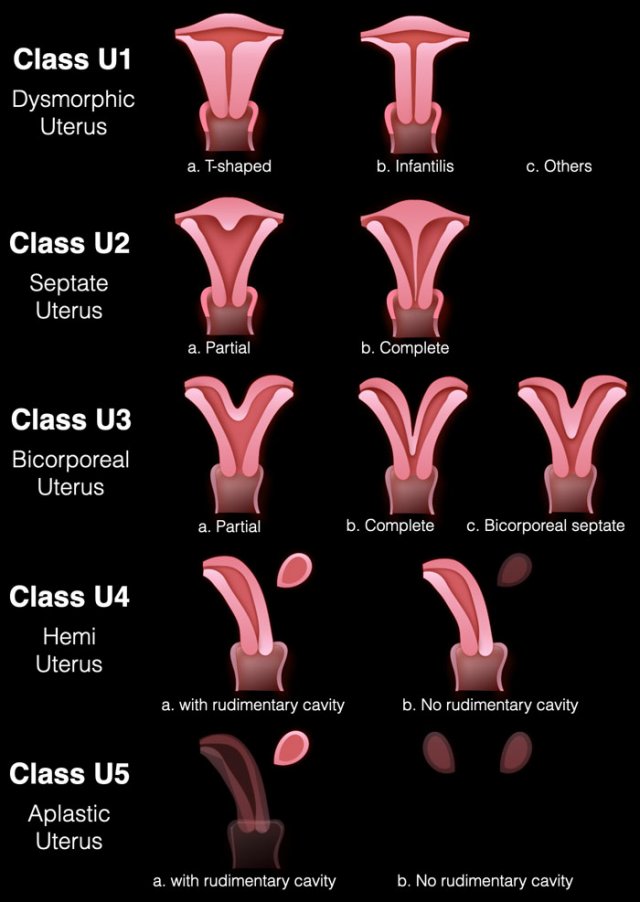
Müllerian duct anomalies
Müllerian duct anomalies, often referred to within the realm of reproductive medicine, are a group of congenital anomalies that result from the abnormal formation, fusion, or resorption of the paramesonephric ducts during embryonic development. These ducts, commonly known as Müllerian ducts, are essential precursors in female fetal development, laying the foundation for the majority of the structures within the female reproductive system. When there’s a disruption in their typical development process, it can lead to various uterine and vaginal anomalies that can have significant implications on human reproduction. For instance, a uterine septum, one of the most common müllerian duct anomalies, refers to a malformation where a wall of tissue divides the uterine cavity either partially or wholly. Other known malformations include the uterine didelphys, where a woman has two separate uterine horns and possibly a didelphys uterus, and cervical agenesis, which refers to the absence of the cervix.
The consequences of müllerian duct anomalies can range from menstrual complications to challenges in achieving and maintaining a pregnancy. For example, an obstructive anomaly, such as a transverse vaginal septum or an obstructed hemivagina, can lead to the accumulation of menstrual blood, causing pain and complications if not diagnosed and treated, often through surgical intervention or vaginal dilation. Women with these conditions might experience issues related to pregnancy loss or preterm birth. Longitudinal vaginal septum and uterine malformations like the uterine didelphys can also present challenges during childbirth. Furthermore, there’s an established association between müllerian anomalies and renal anomalies, making it crucial to evaluate renal anatomy in individuals diagnosed with a müllerian duct anomaly. As the field of reproductive medicine continues to advance, there’s an increasing understanding and ability to address and manage these congenital abnormalities, offering women with müllerian duct abnormalities more comprehensive care and improved reproductive outcomes.
A genitourinary fistula is a permanent opening between the bladder and the vagina, the ureter and the vagina, or the rectum and the vagina. Those fistulas may result from traumatic childbirth, pelvic surgery, trauma or radiation therapy. The symptom of the fistula is loss of urine (vesicovaginal fistula) or stool (rectovaginal fistula) from the vagina.
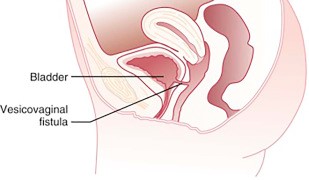
Genitourinary fistulas need to be repaired surgically but surgery may be very complex, and the repair sometimes requires more than one procedure. Some of the fistulas may require grafting (moving) of the surrounding tissues to accomplish the repair. It is very important that genitourinary fistulas are repaired by an experienced surgeon with training in female pelvic medicine and reconstructive surgery (urogynecology).
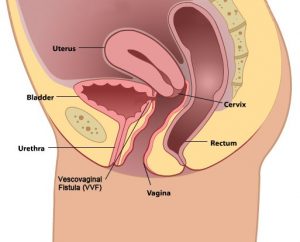
What is Rectovaginal Fistula
A rectovaginal fistula is an abnormal bond between your rectum and vagina that looks like a tunnel opening—while the rectovaginal septum is the thin structure that separates the vagina and rectum. The vaginal tissue damage causes the tissue to die allowing the rectovaginal fistulae to form. Once the rectovaginal fistulae are formed—it lets gas and stool enter your vagina—and inflammatory bowel disease is one of the common causes of it. Other causes of rectovaginal fistulae are:
- Injury during delivery of a baby
- Crohns disease, colorectal disease—and other inflammatory bowel disease
- Radiation injury therapy for gynecologic cancers
- Complications during the surgery in the pelvic area—such as colorectal surgery
The same thing with inflammatory bowel disease—rectovaginal fistulae may cause the patient both physical discomfort and emotional distress—which greatly impacts intimacy and self-esteem.
Symptoms to Look Out For That You Need to Undergo a Rectovaginal Fistula Repair
A rectovaginal fistula repair or rvf repair is a surgical repair where the healthy tissue between your vagina and rectum is stitched jointly to protect and fix the fistula. During the rectovaginal fistulas repair—doctors will need to do an incision or make a cut either between your vagina and anus or inside the vagina—and then the healthy tissue is brought together with several separate layers.
When do you need a rectovaginal fistula repair? Relying on the fistula’s location and size—you may carry minor symptoms such as:
- fecal incontinence or leakage of stool and from the vagina
- Vaginal discharge with a bad odor
- Urinary tract or recurrent vaginal infections
- Discomfort in the vagina, vulva, and perineum (the area between your vagina and anus)
- Pain or discomfort during sexual intercourse
Causes:
Injuries During Childbirth
Obstetric trauma—such as delivery-related injuries to a patient is the most common cause of a rectovaginal fistula. These delivery-related injuries include rips in the perineum—extending to the bowel, an infection of an episiotomy—a surgical cut to widen the perineum during vaginal or normal delivery.
Childbirth injuries—such as obstetric fistula may happen during a long and difficult labor. An obstetric fistula may also involve injury to the anal sphincter. An anal sphincter is the ring of muscle at the end of your rectum. In addition—the anal sphincter is the one responsible for helping you hold in stool.
Crohns Disease
The second most common reason for having a rectovaginal fistula, as well as fistula tract is crohns disease. Crohns disease is an inflammatory bowel disease—in which the digestive tract lining is inflamed (ulcerative colitis).
Radiation Treatment Within Pelvic Area
A patient with a cancerous tumor in their cervix, vagina, rectum, anal canal—or uterus could result in a rectovaginal fistula. Radiation therapy is done by a colorectal surgeon—such therapy can cause a fistula that usually forms around six months to two years after the patient receives the treatment.
Perineal laceration or Any Surgery That Involves your Perineum, Vagina, Anus, or Rectum
Prior to perineal laceration or the surgery in your lower pelvic region—such as the removal of your uterus (hysterectomy)—can lead to the development of a rectovaginal fistula in rare cases. The fistula may form as an outcome of an injury during surgery—leak or infection.
Other Causes
In rare cases—a rectovaginal fistula may be formed by infections in your rectum or anus or rectum—infections of little, swelling pouches in your digestive tract (diverticulitis)—dry and hard stool that gets stuck in your rectum (fecal impaction)—long-term colon and rectum (ulcerative colitis)—and vaginal injury unrelated to delivery.
How Doctors Can Help You:
Physical Exams
Our doctor performs a physical exam on patients in trying to locate the rectovaginal fistula—and our doctor also checks for a possible tumor mass, abscess, or infection. Overall—Arizona Center For Chronic Pelvic Pain’s doctor’s exam includes vaginal, anus—and perineum inspection.
Unless the fistula is located very low in the vagina and can be seen—our doctor may use a speculum for seeing the inside of your vagina. In addition—our doctor might also take a sample of tissue during the procedure for biopsy or lab analysis.
Tests
There are instances when a physical exam may not be enough in finding a fistula—which is why we also offer other tests for locating and evaluating a rectovaginal fistula. These tests also help the medical team in planning for surgery.
Computerized Tomography (CT) Scan
A CT scan done on your pelvis and abdomen has more detail compared to what a standard X-ray does. Through CT scan—it is easier to locate a fistula—as well as determine its cause.
Contrast Tests
In contrast tests, doctors use a barium enema or vaginogram that helps in identifying a fistula—which is located in the upper rectum. Contrast material is used during these tests that show the vagina on an X-ray image.
Blue Dye Test
A blue dye test involves placing a tampon into the vagina—then injecting a blue dye into your rectum. The blue staining on the tampon implies a fistula.
Anorectal Ultrasound
The anorectal ultrasound is a procedure, which uses sound waves in producing a video image of your rectum and anus and the doctor inserts a narrow and wand-like instrument into your rectum and anus. This anorectal ultrasound test can assess the structure of your anal sphincter and may also show a childbirth-related injury.
Magnetic Resonance Imaging (MRI)
MRI is a test that creates images of the soft tissues inside your body. This test can also show the location of a fistula—and whether your other pelvic organs are involved—as well as if you have a tumor.
Anorectal Manometry
This test calculates the sensitiveness—as well as the function of your rectum—which can give more information about the rectal sphincter and your ability to hold stool passage. Anorectal manometry does not locate fistulas—but it may greatly help in planning the fistula repair.
Other Tests
If the doctor suspects you of having inflammatory bowel disease—the doctor may order a colonoscopy to examine your colon. During the procedure—the doctor may take tiny tissue samples for lab analysis—which also helps in confirming chrons disease.
Surgery
Most patients will need to undergo surgery to close or repair a rectovaginal fistula. But, before surgery is done—the skin and the surrounding tissue of the fistula need to be healthy. It has to have no signs of infection or inflammation at all. Most doctors might recommend waiting at least three to six months prior to having the surgery—in order to make sure that the skin and the surrounding tissue are healthy.
Surgery needed to close a fistula is performed by either or both a gynecologic surgeon and a colorectal surgeon. The goal for the surgeons for such surgery is to remove the fistula tract and seal the opening by stitching together healthy tissue.
When Do You Need to See a Doctor?
A fistula could only be the first warning of a more serious problem—for example—an infected—pus-filled area (abscess) or cancer. Reading about the symptoms in the health library is not enough if the symptoms persist. Make sure to see and consult your doctor if you are experiencing any symptoms or signs of a rectovaginal fistula and bring your medical records with you if you have any.
Consult with Arizona Center For Chronic Pelvic Pain—and we’ll identify the cause of the fistula and determine the right treatment plan for you.
Contact our office at 480 599-9682 or email [email protected] to learn more about available treatments.
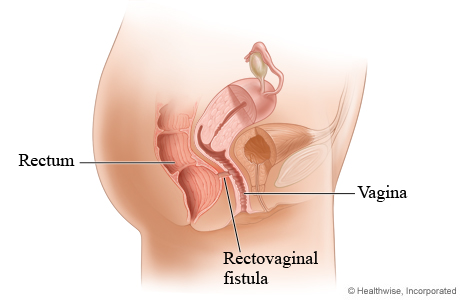
What is Rectovaginal Fistula?
A rectovaginal fistula is a medical condition characterized by an abnormal connection or passage between the rectum and the vagina, known as the fistula tract. This condition, often referenced in health libraries and by healthcare professionals, can result from various causes, including obstetric trauma during childbirth, tissue damage from radiation therapy, complications from surgeries such as open hysterectomy, and inflammatory bowel diseases like Crohn’s disease and ulcerative colitis. Among the spectrum of genitourinary fistulas, which include vesicovaginal and enterovaginal fistulae, the rectovaginal variant presents with distinctive rectovaginal fistula symptoms. These symptoms may include fecal incontinence, where stool might leak into the vagina, frequent vaginal infections due to the continuous presence of fecal matter in the vaginal area, and the passage of gas from the vagina during a bowel movement. Additionally, patients might notice an offensive odor emanating from the vaginal area, originating from the fistula tract, which can significantly impact their quality of life.
Addressing rectovaginal fistulae requires an in-depth understanding of the condition basics and a thorough diagnostic approach. Advanced practitioners or health care providers typically begin with a physical examination of the pelvic area and may recommend imaging studies like a CT scan to visualize the fistula’s exact location and the extent of the tissue breakdown. In cases where the condition is suspected to be a result of inflammatory diseases like Crohn’s disease, confirming the underlying medical condition is crucial before embarking on treatment. The World Health Organization and other prominent health bodies have highlighted the importance of early diagnosis and intervention. The primary treatment for this ailment is rectovaginal fistula repair, which involves surgical closure of the abnormal connection, ensuring that the healthy tissue surrounding the fistula tract is preserved. In cases like the colovaginal fistula, which involves the colon and the vagina, or the vesicovaginal tract fistulas, which concern the bladder and the vagina, the repair approach might differ. Regardless of the type, timely consultation and intervention by a qualified health care provider are essential to ensure optimal patient outcomes and reduce the risk of complications such as tissue breakdown, infection, and persistent urinary or fecal incontinence.
Ovarian Remnant Syndrome (ORS) is a rare medical disorder that develops when ovarian tissue is left behind following ovarian surgery, such as having undergone oophorectomy. (complete removal of one or both ovaries). This can result in several symptoms, such as chronic pelvic pain, menstrual abnormalities, and infertility. ORS might be difficult to identify because its symptoms can resemble those of other gynecological conditions.
ORS is most frequently caused by inadequate ovarian tissue excision during surgery. Sometimes, the surgeon may leave behind a small portion of ovarian remnant tissue, which may cause problems as it grows. Adhesions, scar tissue, and endometriosis may also contribute to ORS.
Despite its rarity, ORS can substantially influence a woman’s quality of life. Women who have previously undergone ovarian surgery must be aware of the symptoms of ORS and seek medical assistance if they have pelvic pain or monthly irregularities. By recognizing the causes and symptoms of ORS, women can collaborate with their healthcare providers to achieve an accurate diagnosis and the most effective therapy.
Symptoms of Ovarian Remnant Syndrome
Ovarian Remnant Syndrome (ORS) symptoms can vary significantly and may be unique for each woman. Infrequent menstrual cycles, pelvic pain, and infertility are some of the most frequent symptoms of ORS.
Irregular Periods
Women with ORS may suffer alterations in their menstrual cycle, including irregular periods, excessive bleeding, or spotting. This can occur when ovarian tissue continues to generate hormones, resulting in hormonal abnormalities.
Pelvic Pain
Pelvic discomfort is a typical symptom of ORS and can fluctuate from mild to severe in intensity. The discomfort may be persistent or intermittent, localized to the pelvis or radiating to the lower back or thighs.
Infertility
ORS can also lead to infertility. The presence of ovarian tissue might hinder ovulation and egg release, making pregnancy difficult for women. In some instances, ovarian tissue may generate hormones that disrupt the menstrual cycle and impair fertility.
Other Symptoms
Other symptoms of ORS include bloating, constipation, painful sexual relations, and urinary urgency or frequency. However, it is crucial to note that some women with ORS may exhibit no symptoms, making the disorder difficult to identify.
If a woman develops any of these symptoms following ovarian surgery, she must seek immediate medical assistance. At AZCCPP, we are committed to providing the highest level of care. If you or someone you know has any of these symptoms, we can help.
An accurate diagnosis is necessary for correct therapy of ORS and to alleviate symptoms that may be harming a woman’s quality of life. ORS may be treated with hormone medication, surgery to remove ovarian tissue, or a combination.
Tips for Managing ORS
Managing Ovarian Remnant Syndrome (ORS) can be difficult, but several techniques can help
ease symptoms and enhance the quality of life. These include lifestyle modifications, pharmaceutical therapies, and surgical intervention procedures.
Lifestyle modifications such as maintaining a healthy weight, being active, and minimizing stress may help manage ORS symptoms. Women with ORS may also benefit from avoiding bladder- and bowel-irritating foods and beverages, such as coffee, alcohol, and spicy meals.
Medications can be beneficial in treating ORS symptoms, including discomfort and irregular periods. Hormonal therapy treatment, such as birth control pills or progesterone therapy, can help regulate the menstrual cycle and alleviate hormonal imbalances. Nonsteroidal anti-inflammatory medicines (NSAIDs) can help reduce pelvic pain.
In certain instances, surgical excision of ovarian tissue may be required to treat the symptoms of ORS. This treatment, known as an ovarian remnant excision, entails the removal of any residual ovarian remnant tissue to limit additional hormone production and lower the risk of recurrence.
Women with ORS must collaborate closely with their healthcare professionals to establish the most effective treatment based on their specific symptoms and needs. Important follow-up appointments are necessary to monitor symptoms and modify treatment as necessary.
In addition to these therapeutic alternatives, women with ORS may benefit from seeking the support of other women who have faced similar obstacles. Support groups and online forums can provide a safe and empathetic environment for sharing experiences, posing questions, and locating resources to manage the disease.
Types of Surgery Available for Treatment
Among the principal therapeutic options for Ovarian Remnant Syndrome (ORS), surgery can effectively alleviate symptoms and lower the chance of recurrence. Depending on the severity of symptoms and the amount of ovarian tissue that must be removed, numerous surgical treatments exist for treating ORS.
Ovarian Remnant Excision
Excision of ovarian remnants entails removing any remaining ovarian tissue following a previous surgery. Typically, the surgeon will use laparoscopic procedures to remove the ovarian tissue through small abdominal incisions. Ovarian remnant excision can help lower ORS-related pain and other symptoms.
Hysterectomy
In some instances, a hysterectomy (complete removal of the uterus) may be indicated to treat ORS. This technique helps lower pain and other symptoms and prevent the recurrence of ORS. Note, however, that if both ovaries are removed, a hysterectomy will result in infertility and menopause.
Salpingo-Oophorectomy
This surgical treatment involves removing one or both ovaries and the fallopian tubes. This surgery is more aggressive and may be advised for women with severe symptoms or a high chance of recurrence. If both ovaries are removed during a salpingo-oophorectomy, the outcome is infertility and menopausal symptoms.
Women with ORS must explore the risks and advantages of each surgical intervention with their healthcare provider and make an informed decision based on their particular requirements and objectives. Recovery time and potential problems will vary depending on the type of surgery performed. Women should be prepared to adhere to post-operative instructions and attend follow-up consultations to guarantee the procedure’s success.
How to Cope with ORS
Managing Ovarian Remnant Syndrome (ORS) can be difficult, but there are several measures women can employ to alleviate symptoms and enhance their quality of life. Some coping strategies for ORS are self-care activities, finding emotional support, and being knowledgeable about the condition.
Self-Care Practices
Self-care practices can be an effective means of managing ORS symptoms and enhancing general health. This can include regular exercise, a balanced diet, adequate rest, and relaxation techniques such as meditation or deep breathing exercises to manage stress. Women with ORS may also benefit from avoiding bladder- and bowel-irritating foods and beverages, such as coffee, alcohol, and spicy meals.
Emotional Assistance
Coping with ORS can be emotionally taxing, and women may benefit from finding support from people who can relate. Support groups and online forums can provide a safe and empathetic environment for sharing experiences, posing questions, and locating resources to manage the disease. To manage stress and other emotional issues, women may benefit from speaking with a mental health expert, such as a therapist.
Being Well-Educated
Being well-informed about ORS can empower and aid women in making informed decisions regarding their treatment and care. Women should keep abreast of the most recent research and treatment options for ORS and collaborate closely with their healthcare providers to builda personalized treatment plan that suits their specific requirements and goals.
Women with ORS must actively participate in their care and prioritize their physical and emotional health. By engaging in self-care, finding assistance, and remaining informed, women with ORS can better manage their symptoms and enhance their overall quality of life.
Conclusion
Ovarian Remnant Syndrome (ORS) can result in various symptoms and substantially influence a woman’s quality of life. However, several treatments can be used to effectively manage symptoms and improve overall health, such as lifestyle modifications, medication, and surgery.
Women with ORS must actively participate in their care, prioritize self-care, and seek support
from healthcare practitioners, support groups, and mental health specialists. If symptoms persist, it is imperative to seek expert assistance to determine the underlying source of the symptoms and to build an effective treatment strategy.
With the proper care and support, women with ORS can control their symptoms and attain optimal health and well-being. Our team at AZCCPP helps patients with this condition. We’ll identify the cause and determine your treatment plan. Contact AZCCPP at 480-599-9682 for a consultation.