Vulvodynia treatment remains a complex challenge due to the chronic and enigmatic nature of this condition, which impacts the vulvar area in women and significantly diminishes their quality of life.
Vulvodynia, characterized by chronic vulvar pain, affects a significant portion of the female population, with estimates ranging from 6% to 28% (Bachmann et al., 2006). Nearly half of women experiencing vulvodynia report adverse impacts on their sexual and psychological well-being (Reed et al., 2012).
It is important to note that vulvodynia is a symptom, not a diagnosis, akin to reporting elbow pain. When the pain is experienced specifically at the vestibule, it is termed vestibulodynia, and when localized to the clitoris, it is known as clitorodynia.
This article goes into detail about the many aspects of vulvodynia. It looks at the newest research on treatment options, vulvodynia bands for extra support, and good ways to take care of yourself.
What is Vulvodynia?
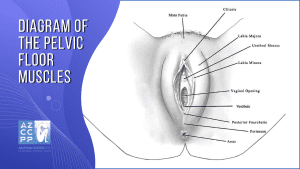
Vulvodynia is a painful disorder that affects the vulva (the outer female genitals). It is known for its potential to substantially impact the quality of life. Since the pudendal nerve supplies vulvar feeling, Pudendal Neuralgia (PN) can overlap with vulvodynia.
This condition is characterized by chronic vulvar pain or discomfort, with symptoms such as burning, stinging, irritation, or rawness. The pain can be localized to one area of the vulva or be more generalized, affecting various parts.
Understanding Potential Risk Factors and Prevalence
The exact cause of vulvodynia is still unknown, but an ongoing study has found some things that may make you more likely to develop this chronic pain condition. Some of the reasons being looked into are genetic predisposition, hormonal imbalances, and inflammatory factors.
Studies that look at how these factors interact with each other hope to figure out the complicated processes that cause vulvodynia, which will help doctors come up with more effective ways to treat each person individually.
Prevalence studies highlight the fact that vulvodynia is common but not always mentioned. A new epidemiological study shows that a lot of women have vulvodynia at some point in their lives. This makes it even more important to raise awareness and take proactive steps to get better health.
Impact on Mental Health and Relationships

Besides physical pain, vulvodynia affects mental health and relationships. Chronic discomfort like vulvodynia can worsen stress, worry, and unhappiness. Vulvodynia can make it challenging to maintain a positive sexual and body image, which can worsen mental health, according to studies.
Vulvodynia can strain relationships, especially intimate ones. Sexual tension and miscommunication emphasize the need for many support systems. This research examines vulvodynia’s psychology. We learn how relationships operate and how to improve communication and understanding.
Symptoms and Types of Vulvodynia
Here are the common symptoms of vulvodynia and its various types:
Elaborating on Symptoms
The symptoms of vulvodynia are diverse and can manifest in various ways. Beyond the hallmark traits of burning, stinging, irritation, or rawness, individuals may experience pain during specific activities such as sitting, exercising, or sexual intercourse. Research emphasizes the subjective nature of these symptoms, highlighting the need for personalized approaches to diagnosis and treatment.
Exploring Different Types of Vulvodynia
Vulvodynia is not a one-size-fits-all condition; instead, it encompasses various subtypes, each with distinct characteristics.
- Provoked Vestibulodynia (PVD): This type is characterized by pain localized to the vestibule, typically triggered by touch or pressure, making activities like intercourse particularly challenging.
- Generalized Vulvodynia: Individuals with generalized vulvodynia experience pain more diffusely across the entire vulvar area, without specific triggers.
- Clitorodynia: This subtype involves pain localized to the clitoral region, posing unique challenges to sexual health and overall well-being.
Not only does studying these subtypes help us learn more about vulvodynia, but it also helps us come up with more effective ways to treat people who have different types of conditions.
Cutting-Edge Vulvodynia Treatment Modalities
A deeper understanding of these factors is crucial for tailoring effective treatment approaches. Here are the current vulvodynia treatment modalities used by experts today:
Medications: A Pillar in Pain Management
Medications have long been a mainstay of vulvodynia treatment, providing relief from pain and discomfort. Traditional pain relievers, such as over-the-counter ibuprofen or acetaminophen, can be effective in managing mild to moderate symptoms. However, for more severe cases, stronger medications, such as opioids or anticonvulsants, may be necessary.
- Antidepressants: Antidepressants, such as tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs), have been shown to be effective in treating vulvodynia, even in women who do not have depression. These medications work by increasing the levels of serotonin and norepinephrine in the brain, which can help reduce pain and improve mood.
- Anticonvulsants: Anticonvulsants, such as gabapentin and pregabalin, are also used to treat vulvodynia. These medications work by calming the nerves that are responsible for pain signals.
- Topical Anesthetics: Topical anesthetics, such as lidocaine or lidocaine-prilocaine, can be applied directly to the vulva to provide temporary relief from pain. These medications work by blocking pain signals from being transmitted to the brain.
- Estrogen Creams: Estrogen creams are a newer treatment for vulvodynia. These creams work by replenishing the estrogen levels in the vulva, which can help improve blood flow and reduce inflammation.
Medications can treat vulvodynia, but they have adverse effects. Common adverse effects include drowsiness, dizziness, nausea, and weight gain. Antidepressants may increase suicide thoughts and acts, especially among younger people. Dizziness, balance issues, and memory loss can result from anticonvulsants. Topical anesthetics can cause burning, stinging, and numbness. Estrogen creams increase blood clots and breast cancer risk.
Physical Therapy Innovations: Targeting Pelvic Floor Dysfunction

Physical therapy has emerged as a promising and effective treatment modality for vulvodynia, particularly for those cases associated with pelvic floor dysfunction. Pelvic floor dysfunction, characterized by muscle tightness, weakness, or incoordination in the pelvic floor muscles, is a prevalent contributor to vulvar pain. Physical therapy aims to address these underlying issues by employing a range of tailored exercises and therapeutic techniques.
Tailored Exercises
Pelvic floor muscle training, a cornerstone of physical therapy for vulvodynia, involves exercises designed to strengthen, relax, and coordinate the pelvic floor muscles. These exercises, typically performed under the guidance of a pelvic floor physical therapist, can help alleviate pain, improve bladder and bowel control, and enhance sexual function.
Therapeutic Techniques
Physical therapists employ a variety of therapeutic techniques in conjunction with pelvic floor muscle training to optimize pain management and overall pelvic health. These techniques may include:
-
Soft tissue mobilization: Manual techniques to release tight muscles and connective tissue around the pelvis and vulva.
-
Biofeedback: A technique that utilizes visual or auditory feedback to train individuals to control their pelvic floor muscles more effectively.
-
Electrical Stimulation: Low-level electrical stimulation is applied to the pelvic muscles to promote relaxation and reduce pain.
Research on Physical Therapy for Vulvodynia
Numerous studies have demonstrated the efficacy of physical therapy in alleviating vulvodynia symptoms. A 2019 systematic review and meta-analysis of 17 randomized controlled trials concluded that physical therapy was significantly more effective than no treatment or placebo in reducing vulvodynia pain.
Potential Risk Factors and Negative Impacts of Physical Therapy
While physical therapy is generally safe and well-tolerated, some women may experience temporary discomfort or pain during or following treatments.
Additionally, some individuals may not experience complete relief from symptoms, and a combination of physical therapy with other treatment modalities may be necessary.
Physical therapy offers a valuable and evidence-based approach to managing vulvodynia, particularly for cases associated with pelvic floor dysfunction. Tailored exercises, therapeutic techniques, and biofeedback have demonstrated efficacy in reducing vulvodynia symptoms and improving overall pelvic health.
Best Physical Therapy for Pelvic Pain in Arizona
A qualified therapist should provide physical treatment for vulvodynia. AZCCPP offers the best pelvic pain treatments in Arizona, with physical therapy being one of Arizona’s best. Complicated pelvic disorders, including chronic pelvic discomfort, require multimodal treatment.
We use your information, clinical knowledge, medical evaluation with Dr. Hibner, and physical therapy evaluation with Tiffany to improve diagnostic and treatment quality and speed, giving you a better picture to make the most personalized care decisions.
Read More About Pudendal Neuralgia Here!
Cognitive-Behavioral Therapy (CBT) for Vulvodynia
The psychological toll of vulvodynia is increasingly recognized, prompting researchers to delve into the benefits of Cognitive-Behavioral Therapy (CBT). Studies indicate that CBT not only helps manage the emotional stress associated with chronic pain conditions but also contributes to tangible improvements in vulvodynia symptoms.
Vulvodynia can have a profound impact on a woman’s emotional well-being. The constant pain, the uncertainty of diagnosis and treatment, and the disruption of intimacy can lead to feelings of anxiety, depression, and isolation.
In recent years, researchers have recognized the significant psychological impact of vulvodynia and have explored the effectiveness of Cognitive-Behavioral Therapy (CBT) in addressing these emotional challenges. CBT is a type of psychotherapy that focuses on identifying and changing negative thoughts and behaviors that contribute to emotional distress.
How CBT Can Help with Vulvodynia
CBT can help women with vulvodynia in several ways:
-
Reducing Anxiety and dDepression: Vulvodynia can exacerbate anxiety and depression, creating a vicious cycle of pain and emotional distress. CBT helps identify and challenge negative thoughts and beliefs that contribute to anxiety and depression, promoting a more positive and hopeful outlook.
-
Improving Pain Management: CBT can help women with vulvodynia develop effective coping mechanisms for managing pain. This includes relaxation techniques, mindfulness exercises, and cognitive strategies for reframing pain perceptions.
-
Enhancing Self-efficacy: CBT empowers women with vulvodynia to take control of their condition, fostering a sense of self-efficacy and reducing feelings of helplessness. This can lead to more active participation in treatment and improved overall well-being.
-
Restoring Intimacy: Vulvodynia can significantly impact sexual function and intimacy. CBT can help couples navigate the challenges of intimacy, addressing communication issues, addressing sexual fears, and promoting a more supportive and understanding relationship.
Clinical studies have indicated that cognitive behavioral therapy (CBT) can treat vulvodynia and its psychological repercussions. CBT reduces pain, improves sexual function, reduces anxiety and sadness, and boosts self-efficacy in vulvodynia patients. These findings make cognitive behavioral therapy (CBT) a crucial adjunct to physical and drug-based vulvodynia treatments.
CBT as Part of a Comprehensive Treatment Plan
CBT is most effective when integrated into a comprehensive treatment plan for vulvodynia. It may be used alongside other therapies such as physical therapy, medications, or biofeedback. Working with a healthcare provider, women with vulvodynia can develop a personalized treatment plan that addresses both the physical and psychological aspects of their condition.
Indeed, CBT has emerged as a valuable tool in managing vulvodynia, not only alleviating pain but also addressing the emotional distress and relationship challenges associated with this chronic condition. CBT can significantly enhance the quality of life for those who suffer from vulvodynia by empowering women to take charge of their health and fostering positive coping mechanisms.
Biofeedback and Neurostimulation
Cutting-edge technologies play a pivotal role in vulvodynia treatment. Biofeedback and neurostimulation techniques, designed to modulate pain perception, showcase promising outcomes. Research in this realm explores the potential of these interventions in enhancing the overall quality of life for women grappling with vulvodynia.
Surgical Interventions: Exploring Vestibulectomy
In severe, localized cases, surgical intervention, particularly vestibulectomy, has been investigated as a viable option. Researchers are looking into the results of this procedure to find out how well it works at helping people with refractory vulvodynia get long-lasting relief.
Vulvodynia Bands: A Supportive Approach
Vulvodynia bands are a type of vaginal dilator that is used to treat vulvodynia. They are made of soft, flexible silicone and come in a variety of sizes. Vulvodynia bands are inserted into the vagina and worn for a few hours at a time. They work by gradually stretching the vaginal muscles, which can help to reduce pain and improve sexual function.
The two main types of vulvodynia bands are:
Vaginal Trainers
Vaginal trainers, also known as Kegel exercisers or pelvic floor trainers, are specifically designed to help women with vulvodynia learn to control and strengthen their pelvic floor muscles. These muscles play a crucial role in supporting the pelvic organs and controlling urination, bowel movements, and sexual function. Weakened or overactive pelvic floor muscles can contribute to vulvodynia pain.
Vaginal trainers are typically used for a few minutes each day, either during Kegel exercises or as a separate training tool. They come in various sizes and shapes, and some may incorporate vibrations or biofeedback to enhance training effectiveness.
Regular use of vaginal trainers can help:
- Improve pelvic floor muscle strength and control
- Reduce vulvodynia pain and discomfort
- Enhance sexual function
- Improve bladder and bowel control
Vestibular Dilators
Vestibular dilators are a type of vaginal dilator specifically designed for women with vestibular vulvodynia. Vestibular vulvodynia is a type of vulvodynia characterized by pain in the vestibule, the area just inside the entrance to the vagina. Vestibular dilators work by gradually stretching the vestibule, which can help to desensitize the area and reduce pain.
Vestibular dilators are typically worn for a few hours each day, starting with a small size and gradually increasing the size as tolerated. The goal is to gradually stretch the vestibule to a pain-free range of motion.
Regular use of vestibular dilators can help:
- Reduce vestibular vulvodynia pain and discomfort
- Improve sexual function
- Enhance desensitization of the vestibule
Choosing the Right Vulvodynia Band
The choice between vaginal trainers and vestibular dilators depends on the specific type of vulvodynia and the individual’s symptoms and needs. If the pain is generalized throughout the vulva, vaginal trainers may be more appropriate. If the pain is localized to the vestibule, vestibular dilators are more suitable.
Vulvodynia bands are generally safe and well-tolerated. However, some women may experience some discomfort or pain when they first start using them. It is important to start with a small size and gradually increase the size as tolerated. Vulvodynia bands should not be used if you have a vaginal infection or if you are pregnant.
Research has shown that vulvodynia bands are particularly useful for individuals experiencing pain during specific activities or prolonged periods of sitting. Available through online platforms and specialized providers, these bands present a convenient and accessible solution for daily symptom management, contributing to an improved quality of life.
It is important to consult with a healthcare provider to determine the appropriate type of vulvodynia band and to receive proper guidance on its use. Healthcare providers can also help monitor progress and adjust the treatment plan as needed.
Here’s a video from the Institute of Pelvic Health that gives a helpful guide to vaginal dilators:
If you are considering using vulvodynia bands, talk to your doctor. They can help you choose the right type of band for you and teach you how to use it properly.
SoLá Pelvic Therapy
SoLá Pelvic Therapy is a non-invasive treatment that utilizes photobiomodulation (PBM) to alleviate pelvic pain associated with conditions like chronic pelvic pain, vulvodynia, and endometriosis. It is a relatively new treatment option that has shown promise in clinical trials.
PBM involves the use of light energy to stimulate cells and tissues. This can help to reduce inflammation, improve blood flow, and promote healing. In the context of SoLá Pelvic Therapy, the PBM energy is delivered to the pelvic floor muscles and surrounding tissues via a laser.
SoLá Pelvic Therapy is typically administered in a healthcare provider’s office. The procedure is painless and takes only a few minutes. Most patients experience no side effects, although some may experience mild discomfort or tingling.
SoLá Pelvic Therapy is often used as part of a comprehensive treatment plan for pelvic pain. It may be used in conjunction with other therapies, such as physical therapy, medications, or counseling.
Here are some potential benefits of SoLá Pelvic Therapy:
- Reduced pelvic pain
- Improved blood flow to the pelvic area
- Decreased inflammation
- Promoted healing of damaged tissues
- Enhanced muscle function
- Improved quality of life
SoLá Pelvic Therapy is a safe and effective treatment option for pelvic pain. If you are experiencing pelvic pain, talk to your doctor about whether SoLá Pelvic Therapy may be right for you.
Please note that SoLá Pelvic Therapy is not a cure-all, and it may not work for everyone. However, it has shown promise in clinical trials and is a valuable treatment option for many women with pelvic pain.
Vulvodynia Self-Care Strategies
Managing vulvodynia effectively also involves adopting various vulvodynia self-care strategies.
Beyond Medical Interventions: The Role of Vulvodynia Self-Care
Comprehensive vulvodynia management extends beyond medical interventions. Research emphasizes the importance of vulvodynia self-care strategies in alleviating symptoms and improving overall well-being.
Irritant Avoidance: Insights from Dermatological Research
Dermatological research emphasizes the significance of avoiding irritants in daily hygiene practices. Scientific evidence supports using mild, unscented soaps and avoiding potential irritants in laundry and clothing detergents.
Clothing Choices: The Impact of Fabric on Comfort
Studies exploring the impact of clothing on vulvodynia symptoms endorse the preference for loose, breathable cotton underwear. The research underscores the role of clothing choices in reducing irritation and promoting comfort.
Lubricants in the Bedroom: A Pleasurable Solution
Research in sexual health highlights the effectiveness of water-soluble lubricants in minimizing discomfort during sexual intercourse for individuals with vulvodynia. Understanding and incorporating these solutions can significantly enhance the intimate aspects of life for those affected.
Stress Management: A Holistic Approach to Vulvodynia Self-Care
The intricate connection between stress and vulvodynia symptoms is underscored in recent research. Regular exercise, relaxation techniques, and stress management strategies are recognized as integral components of a holistic approach to vulvodynia management.
Learn More: Exercises to Avoid if You Have Pudendal Neuralgia
Pudendal Neuralgia Exercises | What exercises should I avoid if I have pudendal neuralgia?