Differentiating Pudendal Nerve Entrapment (PNE) from Other Pelvic Conditions
Diagnosing pudendal nerve entrapment can be challenging because its symptoms often mimic those of other pelvic disorders, such as:
- Piriformis syndrome
- Interstitial cystitis
- Vulvodynia
- Prostatitis
Piriformis syndrome
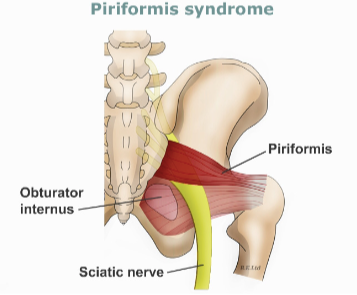
Piriformis syndrome is a condition that can lead to persistent pain, numbness, and tingling sensations in the buttocks, radiating down to the legs. It occurs when the piriformis muscle in the buttocks near the top of the hip joint irritates or compresses the sciatic nerve. Here, we’ll explore piriformis syndrome, beneficial exercises and stretches to alleviate symptoms, and exercises to avoid aggravating the condition.
The piriformis muscle is a small, band-like muscle located in the buttocks, and it is pivotal for lower body movement as it stabilizes the hip joint and lifts and rotates the thigh away from the body. Piriformis syndrome arises when this muscle irritates the adjacent sciatic nerve, resulting in discomfort, tingling, or numbness in the buttocks and along the path of the sciatic nerve descending the lower thigh and into the leg. It’s crucial to understand and address piriformis syndrome promptly as it can significantly impact daily activities and overall quality of life.
Piriformis Syndrome Exercises
Performing the right exercises can help manage piriformis syndrome symptoms by strengthening the muscle and reducing muscle tightness.
- Clamshell Exercise:
– Lie on your side with the hips stacked and knees bent at a 45-degree angle.
– Keeping feet together, lift the upper knee towards the ceiling.
– Perform 2-3 sets of 15 repetitions on each side.
- Piriformis Stretch:
– Sit on the floor with legs stretched out straight.
– Cross the affected leg over the other leg, bending it at the knee.
– Gently pull the knee towards the opposite shoulder until a stretch is felt.
– Hold for 30 seconds and repeat 3 times on each side.
- Bridge Exercise:
– Lie on the back with knees bent and feet flat on the floor.
– Lift the hips towards the ceiling while squeezing the buttocks.
– Hold for a few seconds, then lower the hips to the floor.
– Perform 2-3 sets of 10 repetitions.
Piriformis Syndrome Stretches
Stretching can help relieve the tightness and improve the flexibility of the piriformis muscle. 
- Supine Piriformis Stretch:
– Lie on your back with both feet flat and knees bent.
– Place the ankle of your affected leg over the knee of your other leg.
– Pull the knee of the crossed leg towards the chest gently.
– Hold for 30 seconds and repeat 2-3 times on each side.
- Seated Stretch:
– Sit on a chair, with the affected leg crossed over the knee of the other leg.
– Lean forward gently, keeping the back straight, until a stretch is felt in the buttocks.
– Hold for 30 seconds and repeat 2-3 times on each side.
- Hip Extension Exercise:
– On hands and knees, extend the affected leg straight back.
– Keep the knee straight and avoid arching the back.
– Perform 2-3 sets of 10 repetitions on each side.
Piriformis Syndrome Exercises to Avoid
While exercises and stretches are crucial, some might exacerbate the symptoms of piriformis syndrome. Activities that cause pain, involve vigorous leg movements or put pressure on the piriformis muscle should generally be avoided.
- Deep Squats:
– Squatting too deep can place excessive strain on the piriformis muscle and irritate the sciatic nerve.
- High-Intensity Leg Workouts:
– Exercises involving heavyweights or high resistance can worsen the inflammation and pain.
- Running on Uneven Surfaces:
– Running, especially on uneven terrains, can overwork the piriformis muscle and aggravate symptoms.

Piriformis syndrome, though challenging, can be managed effectively with proper understanding, the right set of exercises, and lifestyle modifications. Incorporating gentle stretches and strengthening exercises can alleviate the symptoms and improve the quality of life. However, recognizing and avoiding movements and activities that can exacerbate the condition is equally important. If the symptoms persist despite these measures, seeking professional medical advice is crucial to prevent further complications and to explore other therapeutic interventions.
Typically, a clinician will diagnose PNE after conducting a thorough physical examination, reviewing the patient’s medical history, and conducting diagnostic tests like:
- Electromyography (EMG) is a non-invasive technique for gauging muscle electrical activity.
- Nerve conduction velocity (NCV) testing, which measures the speed at which nerve impulses travel
- Pudendal nerve block, which involves injecting a local anesthetic near the pudendal nerve to numb the area and help diagnose PNE