Pelvic Congestion Syndrome | What conditions are associated with Pelvic Congestion Syndrome?
Varicose Veins or Vein Engorgement
When blood pools in the pelvic vein or ovarian vein, it may result in enlarged veins, causing pain, tenderness, and redness. Varicose veins usually develop in the legs, calves, and feet, but can also occur in the pelvic region, leading to pelvic congestion syndrome.
Deep Vein Thrombosis (DVT)
DVT occurs when a blood clot forms in a deep vein, and this can occur in the pelvis. The clot then restricts blood flow, which in turn causes pain, swelling, and often varicose veins, such as in the left ovarian vein.
Hydro-nephrosis
Compression on the renal vein can affect urine flow and backing up of urine into the left kidney, causing pelvic congestion syndrome symptom. As a result, affected individuals may report chronic pain and frequent urination.
Peripheral Artery Disease (PAD)
Cholesterol and fat can build up in the arteries forming plaque that blocks blood flow. This leads to peripheral artery disease, wherein the reduction of blood flow affects the iliac arteries in the pelvis. Those affected may suffer from pain and cramps. Men may also experience erectile dysfunction.
Who is at Risk for Pelvic Congestion Syndrome?
Since studies have shown a link between pregnancy and pelvic congestion syndrome, women who have given birth are at risk for developing this condition. Women who have had multiple pregnancies (carrying more than one baby, e.g. twins) are even more at risk than those who have had a singleton pregnancy (carrying one baby), as they are more likely to develop pelvic varices or enlarged veins in the pelvic region.
In addition, those who have a history of pelvic congestion syndrome in the family are also at risk. If you are suffering from chronic pelvic pain and believe you might have this condition, get in touch with a qualified healthcare provider like AZCCPP.
Can I manage Pelvic Congestion Syndrome on my own?
While this condition is not fatal, if left undiagnosed or untreated, pelvic congestion syndrome can lead to further health complications like chronic pelvic pain and permanently damaged vein. Only qualified healthcare professionals like our team at AZCCPP can help you manage it properly through treatments such as interventional radiology and ovarian vein embolization.
We strongly advise you to get in touch with us so we can make the right diagnosis and provide the best pelvic congestion syndrome treatment option for your case.
What are Pelvic Varicosities?
Pelvic congestion syndrome is a condition where pelvic veins become engorged and form pelvic varicosities. Pelvic varicosities usually occur during pregnancy and disappear after. In some patients, they remain, causing pelvic congestion syndrome. It may occur after a full-term pregnancy, but also after preterm birth, miscarriage, or even after ectopic pregnancy. The mechanism in which varicosities cause pain is not well understood, but it may be due to stretching of the vein wall, pressure on the surrounding nerves, or changes in tissue pH. Some varicosities occur in the ovarian veins and veins around the uterus but some patients have varicosities in the vulvar area pressing against the nerves innervating the clitoris, urethra, and labia.
Depending on the location of congested veins patients will experience different symptoms. Congestion of ovarian and uterine veins leads to the sensation of heaviness in the pelvis which is worse with sitting and standing for a prolonged time and better with laying down. On top of the sensation of heaviness, there is occasional sharp shooting pain in the lower abdomen usually on the left side lasting several seconds at a time which may occur a few times a day to a few times per week.
Pelvic congestion may be diagnosed on pelvic MRI or ultrasound but the gold standard test for diagnosis is transfundal venogram.
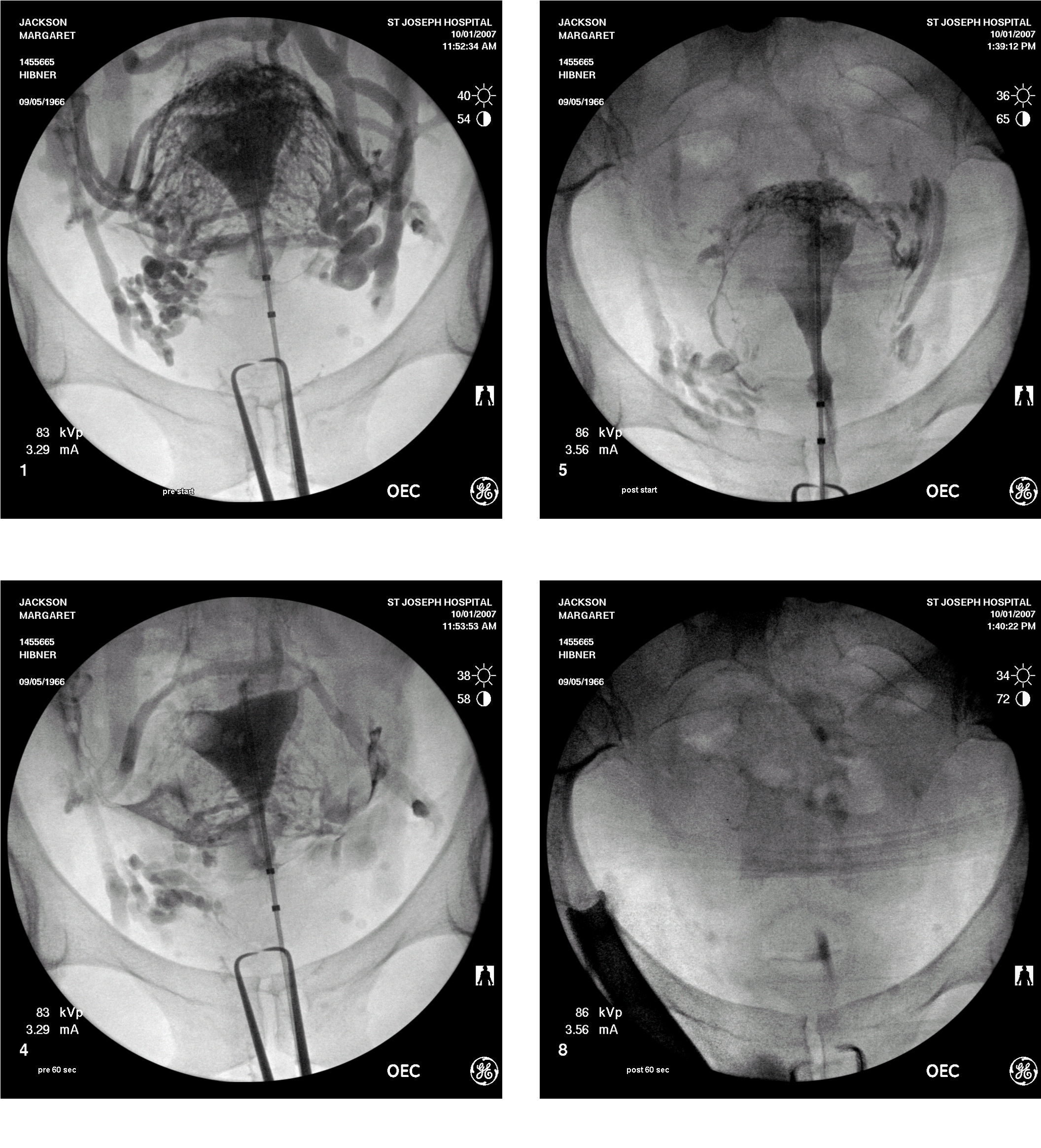
Typical appearance of pelvic congestion syndrome on transfundal venography
Treatment of pelvic congestion may be done by an interventional radiologist who obliterates the congested veins in an attempt to decrease pain. Congested veins may also be closed off surgically by isolating them from the surrounding structures such as nerves and arteries and sealing with a vessel sealing device. An additional benefit of surgical treatment using da Vinci robot over radiological treatment is that surgical treatment of pelvic congestion allows to precisely survey the pelvis and address any other cause of pelvic pain.
Congestion of the veins around the clitoral or perineal branch of the pudendal nerve can only be seen during a special ultrasound examination. This congestion will lead to pain in the clitoris, urethra, and labia and it is worse with sitting and standing. Patients may also experience the sensation of persistent sexual arousal. This type of congestion may be treated by injecting a sclerosing agent into the congested vein in a similar manner as it is done into varicosities in the legs.
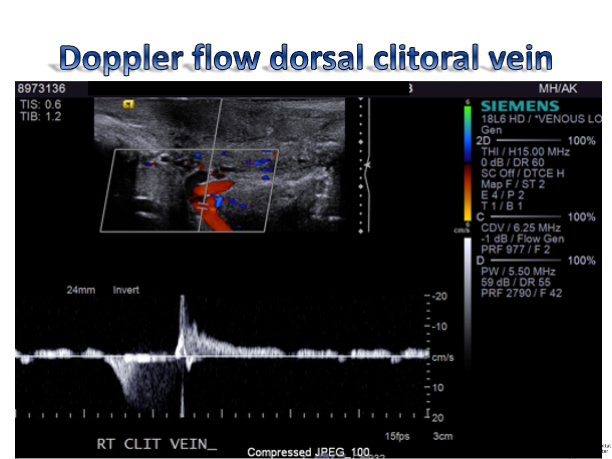
Doppler ultrasound demonstrating congestion in the clitoral vein
What are the Signs and Symptoms of Pelvic Congestion Syndrome?
Again, pelvic congestion syndrome affects everyone differently. It will depend on which pelvic structure the varicose veins are affecting. Here are some signs and symptoms of this condition:
- Your vulva is swollen or you have varicose veins in your genital area.
This happens when pelvis varicose veins go out into the vulva or vagina.
- You have an irritable or painful bladder.
When the pelvic varicose veins push on the bladder, you may feel discomfort or pain when urinating.
- You have hemorrhoids.
Pelvic varicose veins that go into the anus and around the back of the passage may result in bleeding, discomfort, or pain in this area, especially when passing stool.
- You have an irritable bowel.
When the pelvic varicose veins push on the bowel, you may experience symptoms similar to irritable bowel syndrome (IBS): bloating, gas, abdominal pain, cramping, diarrhea, and constipation.
- You experience discomfort or pain during and after sexual intercourse.
This is due to the pelvic varicose veins pushing on the gynecological organs.
- Your pelvic pain worsens during your menstrual cycle.
When the weight of the blood in the veins pushes down on the pelvic floor, you may feel an unusual level of discomfort during your period. You may also experience abnormal bleeding.
- Your pelvic pain worsens throughout the day, especially after physical activities.
Usually, the pain intensifies after sitting or standing for too long, or after physical exercise such as walking, jogging, and lifting weights.
- You feel exhausted.
PCS can be just as draining emotionally as it is physically due to the accompanying
discomfort or pain. Hence, many women claim they also suffer from fatigue and even
mood swings.
Since various conditions exhibit the same signs and symptoms as pelvic congestion syndrome, it is important to consult with a trusted physician for accurate diagnosis and proper treatment.
What Causes Pelvic Congestion Syndrome?
Normally, the arteries send blood from the heart to the rest of the body. Then, the veins send blood from the body back to the heart. This flow is made possible by valves within the veins, which keep the blood from going into reflux or flowing backward.
When the veins become dilated, the valves do not close properly. Reflux then occurs, which leads to pooling of blood within the affected organ–in this case, the pelvis. This results in varicose veins and pelvic congestion syndrome.
While the reason for this condition is unknown, most people who suffer from it are women between the ages 20 and 45 who have had previous pregnancies. One theory suggests that the following can cause pressure within the ovarian veins, leading to vein dilatation:
- Age (particularly during childbearing years)
- Genetics
- Polycystic ovaries
- Retroverted uterus
- Anatomic changes in the pelvic structure due to pregnancy
- Hormonal changes due to pregnancy
- Hormonal dysfunction due to pregnancy
- Weight gain due to pregnancy
- Fluid buildup due to pregnancy
- Increase of blood volume due to pregnancy
- Increase of estrogen due to pregnancy
How Can You Avoid Pelvic Congestion Syndrome?
Since the cause of pelvic congestion syndrome remains unclear, it is not always possible to avoid this condition. However, the risk may be reduced by doing the following:
- Eat a healthy diet
- Exercise regularly
- Quit smoking
- Maintain a healthy weight
- Maintain a healthy body mass index (BMI)
- Wear compression garments during pregnancy
- Wear compression garments on a routine basis after pregnancy
Pelvic Congestion Syndrome in Pregnancy
When a pregnant woman suffers from pelvic congestion syndrome, symptoms usually worsen as the baby grows. The baby’s weight and size exert pressure on the varicose veins of the pelvis, causing great discomfort or pain. The pain may be a dull ache, throbbing, or sharp.
Sitting or standing for a long time can cause the pain to worsen at the end of the day. The best way to relieve it is by lying down. Additionally, every subsequent pregnancy may also worsen the pain.
Outlook
Pelvic Congestion Syndrome may not be fatal, but it can greatly affect your quality of life. For instance, symptoms like hemorrhoids, pelvic pain, and fatigue can take a toll on your physical, mental, and emotional wellbeing.
Fortunately, the symptoms can be minimized and managed with treatments. Your physician might also recommend counseling to help you cope with chronic pain associated with this condition.
To know your treatment options, consult with your doctor.
If you or someone you know has pain that started after pregnancy and has symptoms of pelvic congestion, call our office at 480-599-9682 or email [email protected] to learn more about available treatments.
