Pudendal Nerve Entrapment | Understanding the Causes, Symptoms, and Treatment
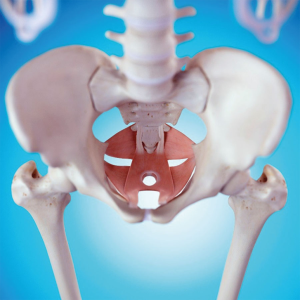
Pudendal Nerve Entrapment, a condition that affects the pudendal nerve in the pelvic region, can produce chronic pain and interfere with daily activities. This post aims to provide valuable insights into understanding the condition, recognizing its symptoms, diagnosing and treating it, implementing lifestyle modifications, and adopting preventative measures for long-term management.
Understanding Pudendal Nerve Entrapment
What is Pudendal Nerve Entrapment?
As mentioned, pudendal nerve entrapment (PNE) is a chronic pain condition caused by irritation or compression of the pudendal nerve. The pudendal nerve is the primary nerve responsible for movement and sensation in the pelvic area, which includes the genitalia, rectum, and bladder. PNE can result in a variety of symptoms, such as:
- Pain in the buttocks, perineum (the area between the genitals and anus), and genitals
- Numbness or tingling in the same areas
- Difficulty with urination or bowel movements
- Pain during sex
- Pain when sitting
Causes and Risk Factors
Although it is not understood what causes PNE, here are some things that can put you at a higher risk of being diagnosed with it:
- Injury to the pudendal nerve during childbirth or surgery
- Repetitive strain injuries, such as from prolonged sitting or cycling
- Structural abnormalities of the pelvis, such as a narrowing of the sacrospinous ligament
- Inflammatory conditions, such as arthritis or endometriosis
- Tumors or cysts in the pelvic region
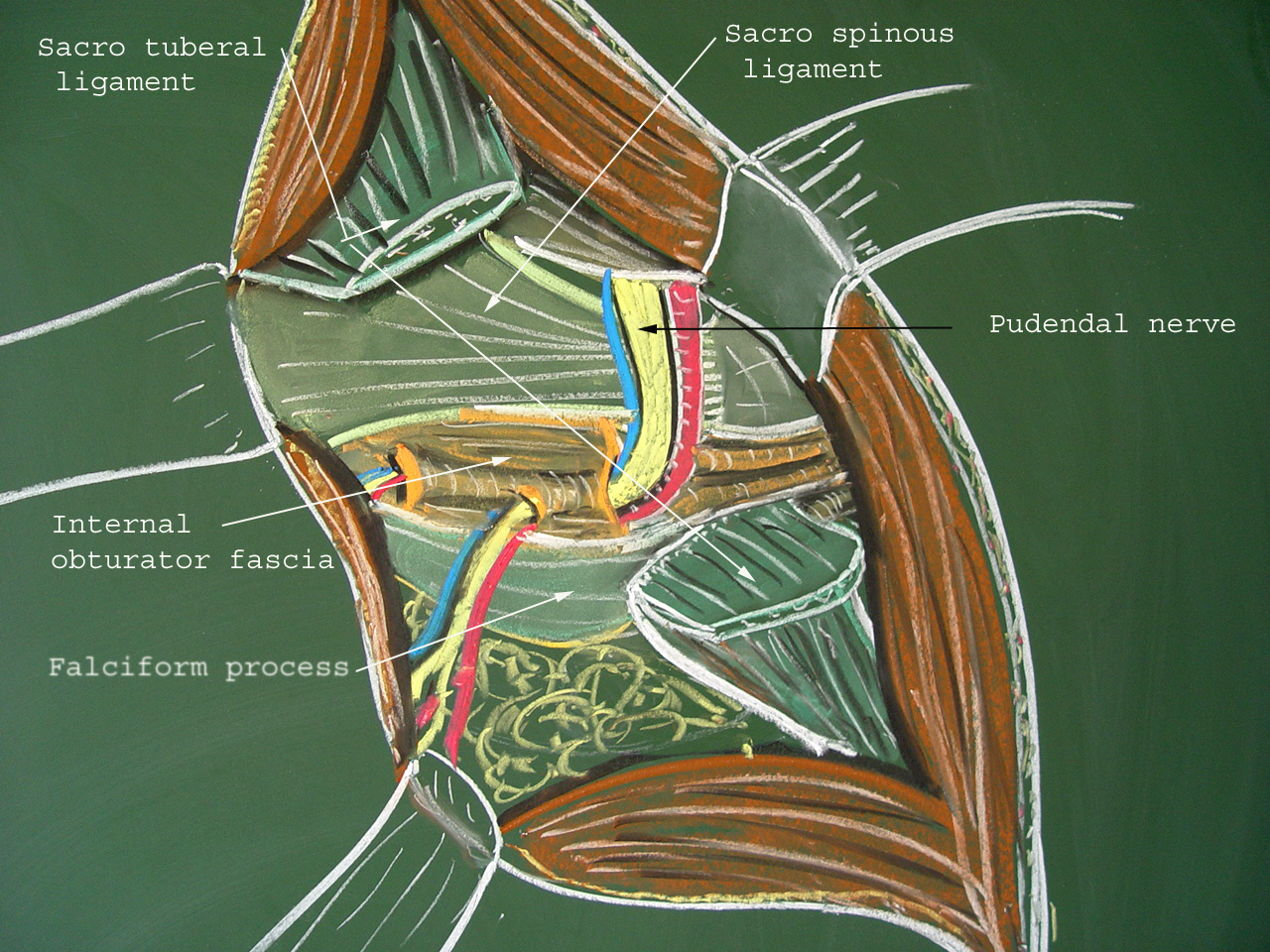
Common Entrapment Sites
The pudendal nerve can become entrapped in various areas, including:
- The greater sciatic notch, where the nerve exits the pelvis
- The Alcock canal is a tunnel in the pelvis that the nerve passes through
- The pudendal nerve fascia, a sheath of tissue that surrounds the nerve
- The perineal body is a small mass of tissue at the junction of the vagina and anus
Differentiating Pudendal Nerve Entrapment from Other Pelvic Conditions
Diagnosing pudendal nerve entrapment can be challenging because its symptoms often mimic those of other pelvic disorders, such as:
Typically, a clinician will diagnose PNE after conducting a thorough physical examination, reviewing the patient’s medical history, and conducting diagnostic tests like:
- Electromyography (EMG) is a non-invasive technique for gauging muscle electrical activity.
- Nerve conduction velocity (NCV) testing, which measures the speed at which nerve impulses travel
- Pudendal nerve block, which involves injecting a local anesthetic near the pudendal nerve to numb the area and help diagnose PNE
Treatment for Pudendal Nerve Entrapment
Treatment for PNE is patient-specific, as there is no universally effective method. Some potential methods of treatment are:
- Medications, such as anti-inflammatories, pain relievers, or muscle relaxants
- Treatment with physical therapy can aid in the stretching and strengthening of the pelvic muscles.
- Injections of steroids or botulinum toxin into the pudendal nerve
- Surgery, which may be an option for patients who have not responded to other treatments
Those with symptoms consistent with pudendal nerve entrapment should visit a doctor immediately. Your symptoms and overall quality of life may benefit from prompt diagnosis and treatment.
Symptoms of Pudendal Nerve Entrapment
Recognizing the signs of pudendal nerve entrapment is crucial for an accurate diagnosis and prompt treatment. The following are some general warning signs to keep an eye out for. However, individual manifestations may vary:
Chronic Pelvic Pain
Chronic pelvic pain is a classic sign of pudendal nerve entrapment. This discomfort is often described as a dull ache in the pelvic region that has been going on for more than six months.
The discomfort could be restricted to one area or spread to the thighs, lower back, or both. It can make even simple things like sitting, walking, or having sexual relations very uncomfortable.
Pain during Sitting or Prolonged Standing
Sufferers with pudendal nerve entrapment may feel discomfort over prolonged periods of sitting or standing. The soreness in the pelvic region might be made worse by sitting on hard surfaces or for long periods. This symptom can significantly influence one’s ability to work, interact socially, and enjoy life.
Numbness or Tingling in the Genital Area
Pudendal nerve entrapment can cause numbness or tingling in the vaginal area. The external genitalia, perineum, and rectum are all sensory organs that receive input from the pudendal nerve.
Numbness, tingling, or “pins and needles” might result from nerve endings being crushed or entrapped. These feelings can be fleeting or constant, and they have the potential to disrupt sexual performance and general well-being.
Sexual Dysfunction and its Impact
Sexual dysfunction may be severely affected by entrapment of the pudendal nerve. Reduced libido, erectile dysfunction in men, and other forms of pain or discomfort during sexual engagement can affect both men and women.
These symptoms can put a burden on personal relationships and cause mental anguish. When dealing with sexual health difficulties, consulting with a healthcare expert who can provide guidance and appropriate treatment options is essential.
Symptoms of Bowel and Bladder Issues
Bowel and bladder problems are additional symptoms of pudendal nerve entrapment. Some people may have increased frequency, urgency, or incontinence of the urine or bowel systems.
These symptoms can cause severe disruptions in everyday life and must be managed cautiously. These symptoms may point to pudendal nerve involvement and necessitate evaluation by a medical professional.
Diagnosis and Treatment Options
Diagnostic Methods for Pudendal Nerve Entrapment
The key to successful treatment of pudendal nerve entrapment is a correct diagnosis. To diagnose a patient’s illness and come up with an effective treatment plan, medical practitioners use a variety of techniques.
Physical Examination and Medical History
To make an accurate diagnosis, it is necessary to perform both a physical examination and a detailed review of the patient’s medical history. The doctor will talk to you about your symptoms, their length, and what might be causing them. The examination could include the following:
- Testing the patient’s pelvic muscle strength.
- Feeling for pain or stiffness.
- Gauging their sensitivity in the genital area.
Nerve Conduction Studies: Assessing Nerve Function
The health and efficiency of the pudendal nerve are often assessed with a nerve conduction study. This painless examination evaluates how quickly and powerfully electrical impulses travel through a nerve. Healthcare providers can detect anomalies or entrapment of a nerve by testing its conduction ability.
Electromyography (EMG): Measuring Muscle Activity
Electromyography (EMG) is another diagnostic tool that can be used to evaluate muscle function. Needles of varying sizes are inserted into targeted muscles to record the electrical activity during contraction and relaxation. This evaluation helps detect muscle dysfunction or anomalies that could cause a pinched pudendal nerve.
Diagnostic Nerve Blocks: Confirming the Diagnosis
Medical providers may use diagnostic nerve blocks to confirm a diagnosis of pudendal nerve entrapment. A local anesthetic is given close to the pudendal nerve to evaluate the patient’s response and provide temporary pain relief. The pudendal nerve’s involvement in pain creation would be further supported if the pain dramatically improved following the nerve block.
Non-surgical Treatment Options
Medications for Pain Management
The symptoms of pudendal nerve entrapment can often be alleviated with medication. Non-steroidal anti-inflammatory drugs (NSAIDs), neuropathic pain medications, and muscle relaxants are some pain medications that medical experts may give to assist in alleviating pain and enhance daily functioning.
Physical Therapy and Pelvic Floor Exercises
Physical therapy and pelvic floor exercises are frequently suggested as a non-invasive alternative to surgical intervention. A trained physiotherapist can show patients how to do exercises that strengthen and stretch the pelvic muscles while also helping them relax. All around, pelvic stability and function are enhanced, and muscle tension is eased thanks to these workouts.
Nerve Stimulation Techniques: A Promising Approach
Transcutaneous electrical nerve stimulation (TENS) and pulsed radiofrequency therapy are two examples of nerve-stimulation procedures that can alleviate pain by altering nerve signals. These methods involve using deficient levels of electricity or magnetic fields to stimulate healing and reduce discomfort.
Surgical Interventions for Severe Cases
Decompression Surgery: Relieving Nerve Pressure
Surgical decompression may be an option when conservative measures fail to alleviate symptoms of severe pudendal nerve entrapment. This surgical technique aims to relieve the entrapped nerve so it can function more normally. Neurolysis and neuroplasty are surgical procedures that relieve pressure on the pudendal nerve.
Neuromodulation: Managing Pain Signals
Implanted devices deliver electrical or magnetic stimulation of the afflicted nerves in neuromodulation procedures. Individuals who have not found relief from conventional treatments for pudendal nerve entrapment may find it helpful to try spinal cord stimulation or peripheral nerve stimulation to assist in modifying pain signals.
Nerve Grafting: Restoring Nerve Function
Nerve grafting may be an option in cases of significant injury or compression of the pudendal nerve. The injured section of the pudendal nerve is repaired or replaced during surgery using a nerve graft harvested from another area of the patient’s body. Restoration of nerve function and relief of symptoms are the goals of nerve grafting.
The Value of Integrating Different Treatment Methods
Multidisciplinary care is typically necessary for treating pudendal nerve entrapment. Comprehensive and tailored treatment plans can be provided through the combined efforts of healthcare professionals from various fields, including pain management specialists, physical therapists, psychologists, and surgeons. With this comprehensive strategy, patients have a higher chance of experiencing successful condition management and enhanced quality of life.
Lifestyle Modifications and Self-Care Strategies
Managing pudendal nerve entrapment requires a multifaceted approach, including medical treatment, behavioral changes, and self-care. Individuals’ symptoms, general health, and quality of life can all benefit from the regular use of these techniques. Some valuable approaches are listed below.
Ergonomic Adjustments for Sitting and Standing
The pressure on the pudendal nerve can be relieved by adopting more ergonomic sitting and standing positions. If you have to sit for prolonged amounts of time, try using a cushion or a specific seat pad with a cutout to lessen the strain on your pelvic area. Keep your back straight by sitting up straight, balancing your weight equally, and working at a workstation that allows you to stand up straight.
Pelvic Floor Relaxation Exercises: Strengthening and Relaxing Muscles
Pelvic floor relaxation techniques help reduce stress and enhance the performance of the pelvic floor muscles. The pelvic floor muscles are actively contracted and released throughout these routines.
Kegel exercises, like others, can strengthen the pelvic floor muscles and provide more structural support for the pelvic organs. Consult a pelvic floor physical therapist for guidance on appropriate exercises and techniques.
Stress Management Techniques: Finding Relief
Pudendal nerve entrapment symptoms might be made worse by stress. The detrimental effects of stress on the human body and mind can be mitigated by using stress management strategies.
Deep breathing techniques, meditation, yoga, or simply participating in relaxing hobbies and activities can help. Finding effective methods of relieving stress is crucial if you want to control your symptoms and boost your health.
Diet and Nutrition Tips for Reducing Inflammation
The inflammation and pain caused by pudendal nerve entrapment may be alleviated by adopting a healthy, anti-inflammatory diet. Consume many nutritious foods, such as fresh produce, whole grains, lean proteins, and healthy fats.
To reduce inflammation, reducing or eliminating your consumption of processed foods, sugary snacks, and foods high in saturated fats is best. The advice of a licensed dietician can be tailored to your nutritional requirements.
Prevention and Long-Term Management
Preventative interventions and long-term management tactics can help lower the likelihood of developing pudendal nerve entrapment and improve symptoms, which is not always possible. Preventative measures can improve health and lessen the severity of symptoms associated with pudendal nerve entrapment. Fundamental approaches include the following:
Preventive Measures for Reducing the Risk of Pudendal Nerve Entrapment
Not knowing what causes pudendal nerve entrapment can be frustrating, but there are strategies to lessen your chances. Preventing nerve irritation or compression may be possible by avoiding activities that place undue tension on the pelvic muscles or involve extended sitting on hard surfaces. Safe and correct procedures during childbirth and pelvic region surgery can also help decrease the likelihood of pudendal nerve entrapment.
Regular Exercise and Maintaining a Healthy Weight
Long-term therapy for pudendal nerve entrapment should include regular exercise and keeping a healthy weight. Regular low-impact exercises like swimming, walking, or yoga can benefit strength, flexibility, and blood flow.
These moves help keep your pelvis steady, ease muscle tension, and maintain healthy nerve function. Furthermore, a healthy weight might reduce nerve compression risk by easing the pelvic area strain.
Proper Posture and Body Mechanics: Essential Considerations
Correct posture and body mechanics are necessary for those suffering from pudendal nerve entrapment. The pelvic region is relieved of some pressure when the body is positioned correctly.
It’s best to sit up straight, with your back properly supported. Reducing nerve pressure is also facilitated by avoiding static positions such as prolonged sitting or standing. Avoiding unneeded stress on the pelvic region can be as simple as paying attention to body mechanics when performing everyday tasks like lifting heavy objects or bending.
Ongoing Self-Care Practices for Long-Term Symptom Management
Consistent self-care behaviors are crucial for symptom management and long-term health maintenance. This involves carrying on with stress management practices, healthy eating habits, and pelvic floor relaxation exercises.
Practicing relaxation techniques regularly, finding stress-relieving activities to partake in, and eating healthily can all aid in symptom management and preventing flare-ups. Ongoing symptom management and high quality of life can be achieved by maintaining regular contact with healthcare professionals, such as pelvic pain specialists or physical therapists, for regular examinations and adjustments to the treatment plan.
Individuals with pudendal nerve entrapment can take charge of their health and well-being using these preventative actions and long-term care options.
Book with us Today!
Pudendal Nerve Entrapment can significantly impact a person’s quality of life. Still, they can find relief and regain control with understanding, a proper diagnosis, and the right treatment.
Patients can empower themselves to long-term management by instituting lifestyle modifications, adopting coping strategies, and practicing preventive measures. Remember that seeking professional assistance and establishing a solid support network is crucial for a better tomorrow.
Are you prepared to manage the discomfort caused by pudendal nerve entrapment? Check out our website for helpful self-care tips and exercises. See us now to get started on the path to relief and a better way of life.
More About Pudendal Neuralgia & Pudendal Nerve Entrapment
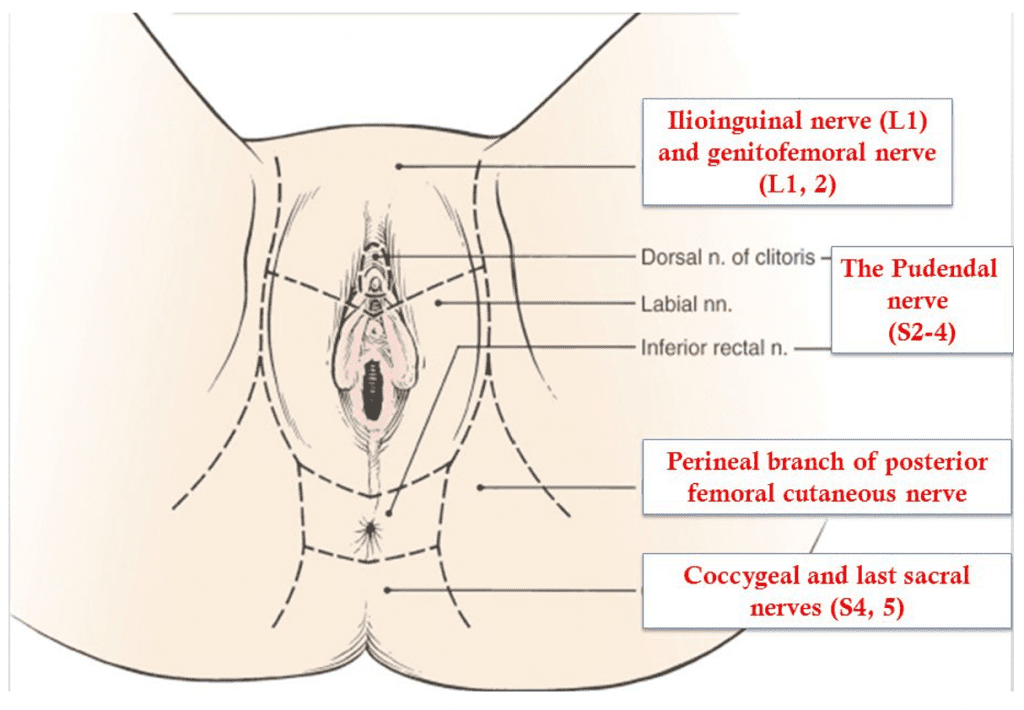
Innervation of the perineum
Pudendal nerve entrapment is almost always caused by some traumatic event to the pelvis. This may be pelvic surgery (with or without mesh), difficult childbirth, athletic injury, falls, and other accidents. A repetitive injury, such as bicycle seat pressure on the pelvic floor, may also lead to pudendal nerve entrapment (cyclist syndrome).
Diagnosis of pudendal nerve entrapment is not easy and relies heavily on taking a detailed history. Pain is located in the vagina, vulva, clitoris, perineum, and rectum, and it may involve one or all of those areas. Pain is more severe with sitting than with standing or lying down, and sitting on the toilet is generally better than sitting on a chair. Most of the patients with real nerve pain injuries have pain on one side only, or one side is significantly more painful than the other. Chronic Pelvic Pain is generally more severe with urination, bowel movements, and intercourse. Some patients may also have difficulty emptying their bladder (hesitancy) and bowel (constipation). One of the most debilitating symptoms of pudendal nerve entrapment is a sensation of continuous sexual arousal (persistent genital arousal disorder – PGAD). Patients often reduce this sensation by masturbation which only provides temporary relief.
A pioneer in the treatment of pudendal nerve entrapment and my mentor, Professor Roger Robert, has developed Nantes criteria which greatly assist in diagnosing this condition. Studies have shown that patients who more closely meet the criteria have better outcomes from the surgical decompression of the nerve.
Nantes Criteria
| Inclusion criteria |
|
|
|
|
|
| Exclusion criteria |
|
|
|
|
| Complementary criteria |
|
|
|
|
|
|
|
|
| Associated signs |
|
|
|
|
|
|
|
|
|
Inferior rectal nerve
Cutaneous branch of the obturator nerve
Lateral cutaneous branch of iliohypogastric nerve
Femoral branch of genitofemoral nerve
Posterior femoral cutaneous nerve
Lateral femoral cutaneous nerve
Iliohypogastric nerve
Clitoral/perineal nerves
Femoral nerve
Genital branch of genitofemoral nerve
Other nerves innervating the pelvis
Pain in pudendal nerve entrapment is of neuropathic nature, which means that patients feel burning tingling and numbing sensation (paresthesia). Some patients have the sensation of a foreign body located in the rectum or vagina (allotriesthesia) and may describe it as a “red hot poker” in the rectum. Some patients do not experience any chronic pain but have complete or partial numbness in the area of innervation of the pudendal nerve.
Additional tests such as magnetic resonance neurography (MRN), pudendal nerve motor terminal latency (PNMTL), another electrophysiologic testing, or sensory threshold testing are generally not accurate enough to diagnose pudendal nerve entrapment. A CT-guided pudendal nerve block is a part of Nantes criteria, and an important step in the diagnosis and treatment of pudendal nerve entrapment. Lack of relief of pain immediately after a CT-guided pudendal nerve block means that pain originates in another structure or is transmitted by a different nerve other than pudendal.
Conservative treatments of pudendal neuralgia consist of:
- Avoidance of additional injury – patients need to immediately stop the activities that lead to injury of the nerve in the first place. For example, if nerve pudendal neuralgia was caused by riding a bicycle, the patient has to immediately stop cycling. Of course, this cannot be done in cases where the patient developed pudendal neuralgia as a result of surgery or childbirth
- Protecting the nerve by using sitting cushions, zero gravity chairs, or kneeling chairs
- Medications including oral medications and vaginal/rectal suppositories
- Appropriate pelvic floor physical therapy (to minimize pelvic floor muscle spasm)
- Botulinum toxin A injections to pelvic floor muscles (to minimize pelvic floor muscle spasm)
- Pudendal nerve blocks using CT, ultrasound, or in some cases unguided transvaginal blocks
- Pudendal nerve injections with amniotic fluid and liquified amniotic membrane
- Ablation procedures – pulse radiofrequency ablation (pRFA) and cryoablation
- Nerve stimulators and spinal cord stimulators
- Surgical decompression of the nerve. Pudendal nerve decompression can be done using several different approaches: transgluteal, transischorectal, transperineal, and laparoscopic/robotic.
The transgluteal approach is an original technique described by Professor Roger Robert in Nantes, France, and very significantly modified by me. This approach offers by far the best access to the pudendal nerve, therefore allowing for the most complete decompression. One of the earlier drawbacks of the technique was cutting of the sacrotuberous ligament which in some cases could lead to pelvic instability. The risk of that instability was eliminated when I began repairing the sactotuberous ligament. Cutting of that ligament allows access to the nerve and frees it from the scar tissue or surgical materials, but after nerve decompression is accomplished sacrotuberous ligament should be repaired.
Other modifications that I have introduced to the pudendal neurolysis surgery were:
- Use of surgical microscope for better visualization of the nerve and surrounding structures
- Use of Nerve Integrity Monitoring System (NIMS monitor) to aid with identification of pudendal nerve. It is especially helpful in cases when the nerve is significantly scarred, and in cases of repeat surgery.
- Use of a pain pump that delivers a local anesthetic to the nerve for about seven days after surgery. This decreases pain levels and is thought to reverse central sensitization (memory of pain in the brain). This step may lead to faster recovery and resolution of pain after surgery.
- Nerve wrapping with an adhesion prevention barrier decreases the risk of scarring or re-scarring of the nerve after surgery. Several years ago, I switched from regular nerve wraps to wrapping the nerve with an amniotic membrane product. In addition to anti-adhesion (anti-scarring) properties, the amniotic membrane contains nerve growth factors that promote nerve healing. It also may have the ability to attract your own body’s stem cells close to the nerve, which further helps with nerve regeneration.
- Use of suction dressing after the closing of the skin to minimize the risk of wound infection
The microscope used for transgluteal pudendal surgery. On the left of the screen NIMS monitor used for monitoring the nerve during surgery
Laparoscopic/robotic procedure is less invasive, but it does not offer as good of access to Alcock’s canal as transgluteal procedure does. It may be effective in cases where the nerve compression is limited to the small area, but the location of compression may be difficult to determine prior to surgery.
In my practice, I perform both transgluteal and robotic nerve decompression procedures, but I believe that since the transgluteal technique offers better access and allows for decompression of the larger part of the pudendal nerve, it should be a preferred approach. Even though the recovery time is longer compared to the laparoscopic procedure, the benefits of more complete nerve decompression are very important when considering the choice of surgery.
Overall, the results of surgery show that the majority of patients have significantly decreased pain, and benefit from pudendal nerve decompression procedures.
If you or someone you know experiences pain with sitting in the clitoris, vulva, penis, scrotum, perineum, or rectum, call 480 599-9682 or email [email protected] to learn more about available treatments.
View of the pudendal nerve through the microscope (nerve in the blue rubber band – vessel loop)
What to expect before and after transgluteal nerve decompression surgery
1. Prior to surgery Dr. Hibner and his team will use some or all available non-invasive methods to help you with your pain. They may include physical therapy, suppositories, oral medications, nerve ablations, injections of amniotic fluid/membrane products.
2. Decision for the surgery is made together by the patient and Dr. Hibner. It is based on all the information from the patient’s history, exam, radiology results, any additional testing. Also, the fact that all offered conservative treatments have failed is taken into account when deciding on surgery.
3. Transgluteal pudendal nerve decompression is Dr. Hibner’s preferred way to free up the nerve from scar tissue but in certain cases robotic approach or highly selective approach to the pudendal nerve, branches may also be chosen.
4. Prior to the surgery please follow all the pre-operative instructions which will be given to you during the visit
5. For the transgluteal decompression surgery you will be positioned on your abdomen (prone) and the incision will go on the buttock on the operated side. It will measure anywhere from 2 to 4 inches.
6. When you wake up from surgery in the recovery area you will have a catheter in your bladder, a pain pump dripping local anesthetic on your nerve, and negative pressure dressing on the skin over the incision. You will receive a bag to wear over your shoulder for the pain pump and device providing suction to the dressing). It is very important to be gentle with the pump to avoid dislodging the catheter. If the pain pump catheter is dislodged, it cannot be replaced.
7. You should feel numbness in the area of the pudendal nerve (where the pain was before surgery) but the incision over the buttock will be quite tender. Pain pump medication does not reach the muscles or skin of the buttock, and it is only meant to provide pain relief in the nerve.
8. Most patients spend one night in the hospital. A very rare two-night stay is required
9. You should be active and try to walk with support the next day after surgery. This prevents a loss of muscle and could also decrease the risk of nerve scarring. Please be very careful when moving and walking not to pull the pain pump.
10. You will be discharged home with pain medications and instructions on how to use the pain pump and negative pressure dressing. You may need to return to the clinic for the dressing and pain pump removal, or we will instruct you how to do it yourself. When the pain pump comes out your pain may increase until the nerve begins healing.
11. You can shower 2 days after surgery. Try to avoid making the area of the incision wet. You can wrap that area with a large garbage bag for the time of surgery. Water is not going to contaminate the incision but may make the adhesive covering the pain pump catheter wet leading to the earlier removal of the pump.
11. Most patients can travel within 5-7 days after surgery but a longer stay is encouraged before traveling back home.
12. You can resume the activity after surgery but avoid doing things that significantly increase your pain. Sitting should be avoided. If surgery was done on one side only try to sit on the opposite buttock.
13. Do not flex your hip(s) over 90 degrees. This may lead to pulling apart the sacrotuberous ligament which was repaired during surgery. This ligament takes approximately 6 months to heal. You should therefore avoid squatting, taking two steps at a time when walking upstairs, etc.
14. You should resume pelvic floor physical therapy approximately 6 weeks from surgery. You will be given instructions for you and your physical therapist regarding recommended therapy.
15. It may take 3-4 months to start feeling the improvement in pain. It is normal to have better and worse days. When you have a better day please be careful not to overexert yourself. Follow the instructions of your pelvic floor physical therapist on physical activity.
16. Please continue to take all your medications until you are instructed to stop. You can continue vaginal/rectal suppositories, but you should be decreasing the number of narcotic pain medications you take.
17. Generally we do not schedule patients for in-person postoperative visits. Care can be done over the phone or by telemedicine.
18. Maximum healing may take 18 to 24 months from surgery. After 2 years from surgery majority of patients have less pain or no pain. If you continue to be in pain, we will look for other solutions to help you with your condition.
Outcomes
Outcomes of this procedure depend on the causes of nerve compression, the degree to which the nerve was compressed, and how much time elapsed between the injury and surgery. Unfortunately, the degree of nerve damage is difficult to assess before surgery. From my extensive experience of doing hundreds of pudendal decompression surgeries, approximately two-thirds (66%) of patients benefit from this procedure. This number includes all the patients, even those with severe nerve injury. That means that patients with less severe nerve injury may benefit from the procedure even more.

Patient positioned for Pudendal decompression surgery. The incision the buttock marked with a pen. Electrodes are placed for monitoring the pudendal nerve (NIMS monitor).
A little history…
Pudendal neuralgia has been recognized by medicine in the book published in Philadelphia in 1871 – “The Change of Life in Health and Disease”. The knowledge of pudendal neuralgia was almost lost until the late 1980s. French neurologist Dr. Gerard Amarenco reported on a series of patients with “syndrome du cyclist”, the cyclist syndrome which occurs when a pudendal nerve is compressed between narrow bicycle seat and medial surface of ischial tuberosity (sitz bone). The first procedure to surgically decompress the pudendal nerve through transperineal technique (incision around the anus) was described in 1992 by Egyptian surgeon Dr. Ahmed Shafik. Soon after my mentor Professor Roger Robert from Nantes, France described transgluteal pudendal neurolysis – decompression of the pudendal nerve with an approach through the buttock. Professor Robert is not only an outstanding neurosurgeon, but also an anatomist, and this unique combination allowed him to develop the whole new procedure for pudendal nerve decompression.
I graduated from my fellowship in gynecologic surgery at Mayo Clinic in 2003 and opened pelvic pain practice in Phoenix in 2004. I started seeing patients with pelvic pain whose condition could not be explained by any disease known to me. So, in early 2005 I googled the symptoms: perineal/vaginal bringing pain with sitting. Several medical articles showed up, but most of them had one common name as one of the authors: Roger Robert. I then send the letter to Nantes France to Professor Robert if I could come to visit him and learn from him. In the summer of 2005, I traveled to Nantes and worked with Professor Robert for almost 3 weeks assisting him on numerous surgeries and seeing many patients in the office with him. I also worked with wonderful Dr. Jean Jacques Labat, a neurologist who assisted Professor Robert with diagnosing and treating patients before surgery, and with amazing radiologist Dr. Thibault Riant who taught me how to perform CT-guided pudendal nerve blocks. When I returned to Phoenix, I started seeing more and more patients with pudendal neuralgia and pudendal nerve compression, and I performed my first transgluteal pudendal nerve decompression in the fall of 2005. It was in the patient who developed pudendal neuralgia after removal of Bartholin’s gland. She did well after surgery and soon many more patients have followed. From the very first surgery, I started modifying the original procedure developed by my great mentor, Professor Robert. The first modification was repairing of the transected sacrotuberous ligament. There was a concern that leaving this ligament not repaired may cause instability in the sacroiliac joint. So, from the very first patient, I would repair sacrotuberous ligament the same way that an orthopedic surgeon repairs a ligament in the knee. Next, I incorporated the use of a neurosurgical microscope into the procedure. This allowed for significantly improved precision. The next modification was the use of an On-Q pain pump placed next to the nerve towards the end of surgery to provide postoperative analgesia and decrease central sensitization (memory of pain in the brain). The third modification was the incorporation of NIMS (nerve integrity monitoring system) to allow to the identification of the nerve in the setting of significant scarring. The next modification was the use of nerve wrap to prevent the reoccurrence of adhesions. Initially, I was using a collagen nerve conduit but a few years ago I switched to an amniotic membrane which in addition to preventing adhesions also contains factors/chemicals promoting nerve healing. The last major modification was the method in which I cut the sacrotuberous ligament. Cutting it in a Z fashion allows me for better access to the nerve and facilitates the repair at the end of surgery. Up to today, I have done several hundred of those procedures, most likely more than any other provider with exception of my amazing mentor, Professor Roger Robert.

From the left: Dr. Jean-Jacques Labat, me, Professor Roger Robert and Dr. Thibault Riant
For more information visit:
https://www.glowm.com/section_view/heading/pudendal-neuralgia/item/691
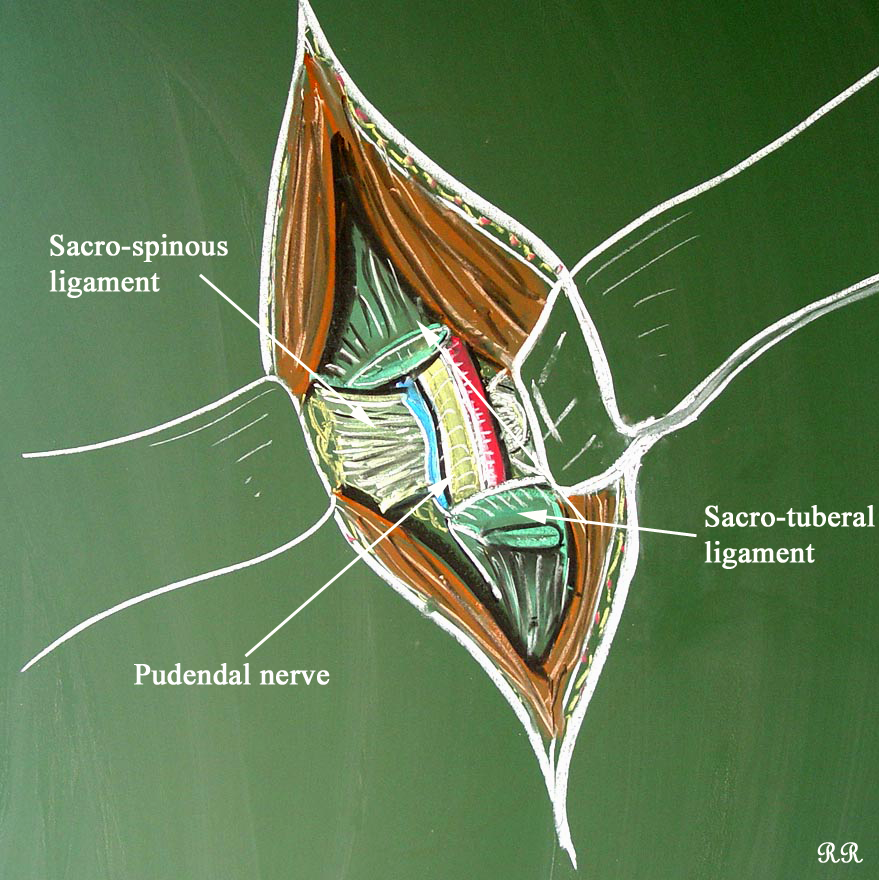
Drawing of the steps of transgluteal pudendal neurolysis by Professor Roger Robert
View of the opened space between the sacrotuberous and sacrospinous ligaments by Roger Robert
One of my numerous publications on pudendal neuralgia
Special thanks
Hard work and knowledge of many, many people went to the development of transgluteal pudendal decompression surgery the way I perform this procedure today. I would like to take this opportunity and thank Professor Roger Robert, Professor Oskar Aszman, Dr. Jamie Balducci, Dr. Jacek Bendek, Dr. Mario Castellanos, Dr. May Nour, Cindy Love, and many others. Big thank you from me and on behalf of my patients whom I was able to help with pain.
Pelvic Pain Frequently Asked Questions:
What is Pelvic Pain?
Pelvic pain in women is a common symptom that accounts for up to 30% of visits to a gynecologist, yet it is thought that close to 70% of cases of pelvic pain are not of a gynecological origin. Chronic pelvic pain is defined as pain that has been present for six months or longer, is localized to the pelvis, and is severe enough to cause functional disability requiring treatment. It is estimated that chronic pelvic pain affects 15% of women in the United States sometime during their lifetime. Yet, almost 60% of those patients do not have a proper diagnosis (and therefore no treatment). This is because this pain usually spans more than one specialty, and treatment requires physicians specifically trained in chronic pelvic pain. Those statistics are even more staggering because over 20% of women with pelvic pain miss work, close to 50% feel depressed, and in 90% of women, it affects their sexual life. Pain during or a complete inability to have intercourse significantly affects personal relations between the patient and her partner and further adds to suffering. Despite the fact that chronic pelvic pain in women is more common than coronary artery disease, asthma, or migraine headaches, very few physicians specialize in its treatment. Pain is often blamed on psychological issues, and patients are often referred to a mental health provider instead of getting treatment for their true, existing disease.
What conditions cause pelvic pain?
Multiple conditions may cause pelvic pain, often coexisting in one patient. Some of the more common conditions are:
- Endometriosis
- Interstitial cystitis/bladder pain syndrome
- Irritable bowel syndrome
- Spastic pelvic floor syndrome
- Adhesions in the pelvis and abdomen
- Pelvic congestion syndrome
- Pelvic nerve neuralgias
- Pain caused by pelvic mesh
The Arizona Center for Chronic Pelvic Pain offers comprehensive treatment for those and many other conditions causing pelvic pain.
What is pudendal neuralgia?
Pudendal neuralgia is a relatively unknown cause of severe pelvic pain.
In my practice, I define it as a pain located in the area of innervation of the pudendal nerve. Pudendal nerve entrapment is an impingement of the pudendal nerve caused by scar tissue, surgical materials, or mesh. Pudendal nerve entrapment is, therefore, one of the causes of pudendal neuralgia. However, other causes, such as inflammation, spasm of the surrounding muscles, or other nerve diseases, may also be reasons for pain.
What is pudendal neuralgia for men?
Pudendal neuralgia is defined as pain in the area of innervation of the pudendal nerve. In men, the areas affected can be the penis, scrotum, perineum, and rectum. Pudendal nerve entrapment is described as compression of the pudendal nerve from ligaments, scar tissue, or surgical materials, which leads to pudendal neuralgia. Some patients with pudendal nerve entrapment experience burning pain, but others may have a sensation of numbness. It may be present on one or both sides, and some patients experience problems with erection and pain with ejaculation. Penile numbness is one of the more frequent signs of pudendal neuralgia in men.
