In the realm of women’s health, mesh-related pain is a complex issue that demands comprehensive understanding and precise solutions. At the core of this matter lies many questions, often unanswered, that can leave individuals grappling with uncertainty and discomfort.
We take it upon ourselves to respond to these concerns in a clear and authoritative manner as experts in women’s health, providing knowledge and direction to help those who are suffering from this condition.
What is Mesh-Related Pain?
Mesh-related pain, also known as mesh complications or mesh-related complications, refers to discomfort or pain experienced by individuals who have undergone surgical procedures involving mesh implants. These implants are commonly used in various medical procedures, including hernia repair and pelvic organ prolapse (POP) repair.
While intended to support and stabilize weakened or damaged tissues, mesh implants can sometimes lead to adverse effects, including pain and discomfort.
Over half of women will develop urine incontinence and prolapse as they get older, have children, or their hormones change. These pelvic floor conditions can be treated with or without surgery. For a long time, patients’ tissue was used in pelvic floor surgeries, which is called “native tissue repair.”
But in 1996, the first polypropylene pelvic mesh was used to treat stress urine incontinence. It quickly took the place of standard surgeries, and mesh-based surgeries became the most common way for women to treat stress urinary incontinence.
Mesh was first used to treat pelvic organ prolapse in 2004, and soon after, the FDA started getting reports of patients who were having problems after this surgery.
In 2008, the FDA sent out the first warning about the risks of pelvic mesh. In 2016, pelvic mesh was reclassified as a type class III device, which means that a lot of study must be done before the devices can be sold.
In 2019, polypropylene mesh for pelvic organ prolapse was taken off the market completely. People who have stress urine incontinence are still treated with polypropylene mesh that is used in retropubic and transobturator slings.
The process of implanting polypropylene mesh to treat incontinence or prolapse goes well for most people, and they don’t have any problems afterward. When complications do happen, they can range from mild discomfort to severe erosion to chronic pelvic pain that is so bad that it makes it impossible to do anything. Some patients also have serious autoimmune reactions to mesh, which can make the terrible pain they are already in even worse.
Common Symptoms of Mesh-Related Pain
Mesh-related pain is often a complex and challenging condition, with symptoms that vary widely in intensity and type. This pain typically occurs when the surgical mesh, often used for treating pelvic organ prolapse or stress urinary incontinence, causes inflammation, nerve damage, or structural complications within the pelvic region.
Here are some common symptoms associated with mesh-related pain:
-
Chronic Pelvic Pain
This is one of the most frequently reported symptoms. Chronic pelvic pain may be constant or intermittent, ranging from dull aches to sharp, stabbing sensations. This type of pain can affect daily activities, making movement and exercise difficult.
-
Pain During Intercourse (Dyspareunia)
Pain during sexual activity is another distressing symptom of mesh-related complications. Dyspareunia can be caused by mesh erosion, scar tissue, or inflammation, leading to discomfort and strain on intimate relationships.
-
Abdominal Pain
Abdominal pain associated with mesh-related issues can extend beyond the pelvic area, sometimes radiating to the lower back or thighs. Without specific treatment, this pain can be challenging to manage because it frequently gets worse with physical activity or prolonged sitting.
-
Recurrent Urinary Tract Infections (UTIs)
The presence of mesh near the bladder can lead to irritation, making recurrent UTIs a common symptom. These infections can cause burning during urination, frequent urges to urinate, and discomfort in the lower abdomen, further impacting daily comfort and health.
-
Pain During Bowel Movements
For some women, mesh placement can lead to discomfort or pain during bowel movements. This can result from pressure on surrounding organs or nerves, causing symptoms similar to irritable bowel syndrome (IBS) and making digestion uncomfortable.
-
Vaginal Discharge or Bleeding
Mesh erosion into the vaginal wall can lead to unusual discharge or spotting between periods. A healthcare professional should take immediate action to treat severe mesh exposure in the vaginal tissue, which may result in irritation, infections, and bleeding.
These symptoms can be both physically and emotionally overwhelming, significantly affecting quality of life and mental health. Many women experience anxiety, frustration, and a reduced sense of well-being due to the impact of these symptoms on their relationships, social activities, and overall lifestyle.
Seeking timely evaluation and treatment from specialists experienced in managing mesh complications is essential for alleviating symptoms, restoring function, and enhancing overall quality of life.
Causes of Mesh-Related Pain
The causes of mesh-related pain are multifaceted and can stem from various factors, including:
-
Mesh Erosion or Migration
When the mesh implant moves from its original placement, it can cause irritation and damage to surrounding tissues, leading to pain.
-
Inflammation
The body’s immune response to the mesh material can result in inflammation, causing pain and discomfort.
-
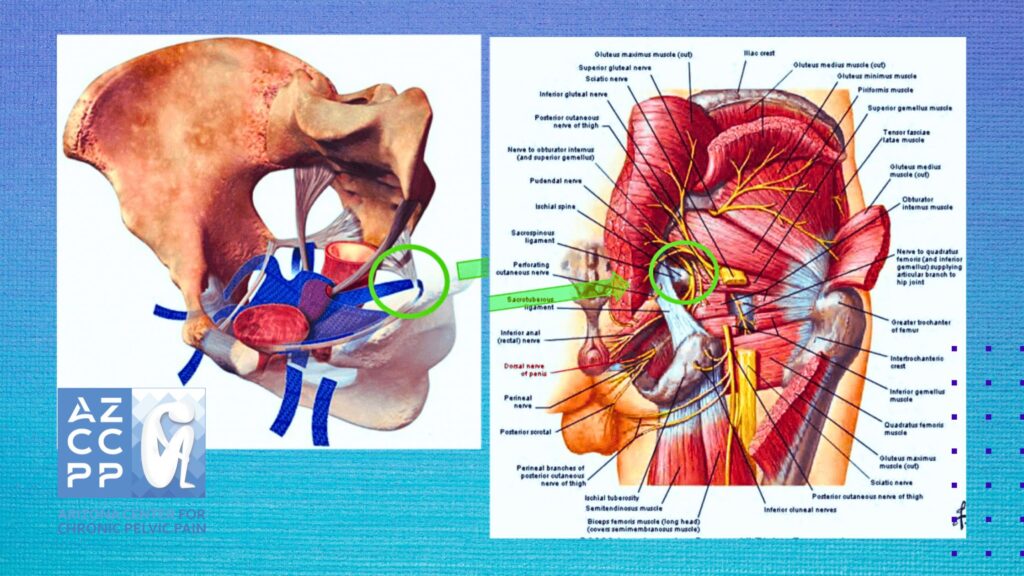
Nerve Damage
Surgical procedures involving mesh implants can inadvertently damage nerves in the surrounding area, leading to chronic pain.
-
Scar Tissue Formation
The body’s natural healing process can result in the formation of scar tissue around the mesh implant, which may contribute to pain and discomfort.
Diagnosis and Treatment Options
Diagnosing mesh-related pain requires a thorough evaluation by a qualified healthcare professional, often involving a combination of medical history review, physical examination, and diagnostic tests such as imaging studies or pelvic exams. Once diagnosed, treatment options may vary depending on the severity of symptoms and individual patient factors. Some common approaches include:
-
Conservative Management
This may include pain management techniques such as physical therapy, medications, and lifestyle modifications to alleviate symptoms.
-
Surgical Intervention
In cases where conservative measures fail to provide relief, surgical removal of the mesh implant may be considered. However, it’s essential to weigh the risks and benefits of surgery carefully and consult with a skilled surgeon experienced in mesh removal procedures.
Seeking Support and Resources

Navigating mesh-related pain can be challenging, but individuals affected by this condition are not alone. There are numerous resources available, including support groups, online forums, and advocacy organizations, where individuals can connect with others facing similar challenges, share experiences, and access valuable information and support.
Conclusion
Mesh-related pain presents a complex and often misunderstood issue for women. By understanding the symptoms, causes, diagnosis, and treatment options associated with this condition, individuals can take proactive steps to manage their symptoms and improve their quality of life.
To ensure thorough care and support for those experiencing mesh-related pain, it is crucial to seek assistance from qualified healthcare professionals and look into available resources.
If you have questions or concerns about mesh-related pain or other related women’s health issues, the Arizona Center for Chronic Pelvic Pain offers expert evaluation and personalized guidance. Contact us at (480) 599-9682 or [email protected] to schedule a consultation.
READ MORE: Comprehensive Guide of Symptoms & Treatments for Vulvodynia
Contact Us for Mesh-Related Pain Treatment for Women

Take control of your health and find relief from mesh-related pain. Connect with us to discuss your symptoms, get answers to your questions, and receive expert guidance for managing this condition. Book a personalized consultation by calling (480) 599-9682 or emailing [email protected]. Let’s work together to bring you comfort, clarity, and a renewed sense of well-being. Visit the Arizona Center for Chronic Pelvic Pain to explore our services and see how we can support your journey.
In addition, check out AZCCPP on YouTube for more questions that need answers with Dr. Michael Hibner.

