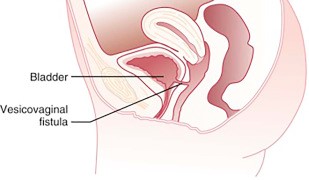
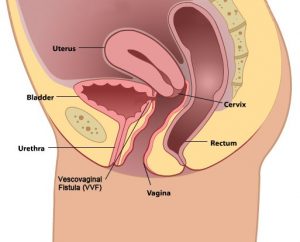
A genitourinary fistula is a permanent opening between the bladder and the vagina, the ureter and the vagina, or the rectum and the vagina. Those fistulas may result from traumatic childbirth, pelvic surgery, trauma or radiation therapy. The symptom of the fistula is loss of urine (vesicovaginal fistula) or stool (rectovaginal fistula) from the vagina.
Genitourinary fistulas need to be repaired surgically but surgery may be very complex, and the repair sometimes requires more than one procedure. Some of the fistulas may require grafting (moving) of the surrounding tissues to accomplish the repair. It is very important that genitourinary fistulas are repaired by an experienced surgeon with training in female pelvic medicine and reconstructive surgery (urogynecology).
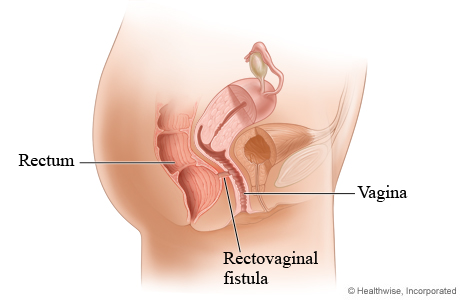
What is Rectovaginal Fistula
A rectovaginal fistula is an abnormal bond between your rectum and vagina that looks like a tunnel opening—while the rectovaginal septum is the thin structure that separates the vagina and rectum. The vaginal tissue damage causes the tissue to die allowing the rectovaginal fistulae to form. Once the rectovaginal fistulae are formed—it lets gas and stool enter your vagina—and inflammatory bowel disease is one of the common causes of it. Other causes of rectovaginal fistulae are:
- Injury during delivery of a baby
- Crohns disease, colorectal disease—and other inflammatory bowel disease
- Radiation injury therapy for gynecologic cancers
- Complications during the surgery in the pelvic area—such as colorectal surgery
The same thing with inflammatory bowel disease—rectovaginal fistulae may cause the patient both physical discomfort and emotional distress—which greatly impacts intimacy and self-esteem.
Symptoms to Look Out For That You Need to Undergo a Rectovaginal Fistula Repair
A rectovaginal fistula repair or rvf repair is a surgical repair where the healthy tissue between your vagina and rectum is stitched jointly to protect and fix the fistula. During the rectovaginal fistulas repair—doctors will need to do an incision or make a cut either between your vagina and anus or inside the vagina—and then the healthy tissue is brought together with several separate layers.
When do you need a rectovaginal fistula repair? Relying on the fistula’s location and size—you may carry minor symptoms such as:
- fecal incontinence or leakage of stool and from the vagina
- Vaginal discharge with a bad odor
- Urinary tract or recurrent vaginal infections
- Discomfort in the vagina, vulva, and perineum (the area between your vagina and anus)
- Pain or discomfort during sexual intercourse
Causes:
Injuries During Childbirth
Obstetric trauma—such as delivery-related injuries to a patient is the most common cause of a rectovaginal fistula. These delivery-related injuries include rips in the perineum—extending to the bowel, an infection of an episiotomy—a surgical cut to widen the perineum during vaginal or normal delivery.
Childbirth injuries—such as obstetric fistula may happen during a long and difficult labor. An obstetric fistula may also involve injury to the anal sphincter. An anal sphincter is the ring of muscle at the end of your rectum. In addition—the anal sphincter is the one responsible for helping you hold in stool.
Crohns Disease
The second most common reason for having a rectovaginal fistula, as well as fistula tract is crohns disease. Crohns disease is an inflammatory bowel disease—in which the digestive tract lining is inflamed (ulcerative colitis).
Radiation Treatment Within Pelvic Area
A patient with a cancerous tumor in their cervix, vagina, rectum, anal canal—or uterus could result in a rectovaginal fistula. Radiation therapy is done by a colorectal surgeon—such therapy can cause a fistula that usually forms around six months to two years after the patient receives the treatment.
Perineal laceration or Any Surgery That Involves your Perineum, Vagina, Anus, or Rectum
Prior to perineal laceration or the surgery in your lower pelvic region—such as the removal of your uterus (hysterectomy)—can lead to the development of a rectovaginal fistula in rare cases. The fistula may form as an outcome of an injury during surgery—leak or infection.
Other Causes
In rare cases—a rectovaginal fistula may be formed by infections in your rectum or anus or rectum—infections of little, swelling pouches in your digestive tract (diverticulitis)—dry and hard stool that gets stuck in your rectum (fecal impaction)—long-term colon and rectum (ulcerative colitis)—and vaginal injury unrelated to delivery.
How Doctors Can Help You:
Physical Exams
Our doctor performs a physical exam on patients in trying to locate the rectovaginal fistula—and our doctor also checks for a possible tumor mass, abscess, or infection. Overall—Arizona Center For Chronic Pelvic Pain’s doctor’s exam includes vaginal, anus—and perineum inspection.
Unless the fistula is located very low in the vagina and can be seen—our doctor may use a speculum for seeing the inside of your vagina. In addition—our doctor might also take a sample of tissue during the procedure for biopsy or lab analysis.
Tests
There are instances when a physical exam may not be enough in finding a fistula—which is why we also offer other tests for locating and evaluating a rectovaginal fistula. These tests also help the medical team in planning for surgery.
Computerized Tomography (CT) Scan
A CT scan done on your pelvis and abdomen has more detail compared to what a standard X-ray does. Through CT scan—it is easier to locate a fistula—as well as determine its cause.
Contrast Tests
In contrast tests, doctors use a barium enema or vaginogram that helps in identifying a fistula—which is located in the upper rectum. Contrast material is used during these tests that show the vagina on an X-ray image.
Blue Dye Test
A blue dye test involves placing a tampon into the vagina—then injecting a blue dye into your rectum. The blue staining on the tampon implies a fistula.
Anorectal Ultrasound
The anorectal ultrasound is a procedure, which uses sound waves in producing a video image of your rectum and anus and the doctor inserts a narrow and wand-like instrument into your rectum and anus. This anorectal ultrasound test can assess the structure of your anal sphincter and may also show a childbirth-related injury.
Magnetic Resonance Imaging (MRI)
MRI is a test that creates images of the soft tissues inside your body. This test can also show the location of a fistula—and whether your other pelvic organs are involved—as well as if you have a tumor.
Anorectal Manometry
This test calculates the sensitiveness—as well as the function of your rectum—which can give more information about the rectal sphincter and your ability to hold stool passage. Anorectal manometry does not locate fistulas—but it may greatly help in planning the fistula repair.
Other Tests
If the doctor suspects you of having inflammatory bowel disease—the doctor may order a colonoscopy to examine your colon. During the procedure—the doctor may take tiny tissue samples for lab analysis—which also helps in confirming chrons disease.
Surgery
Most patients will need to undergo surgery to close or repair a rectovaginal fistula. But, before surgery is done—the skin and the surrounding tissue of the fistula need to be healthy. It has to have no signs of infection or inflammation at all. Most doctors might recommend waiting at least three to six months prior to having the surgery—in order to make sure that the skin and the surrounding tissue are healthy.
Surgery needed to close a fistula is performed by either or both a gynecologic surgeon and a colorectal surgeon. The goal for the surgeons for such surgery is to remove the fistula tract and seal the opening by stitching together healthy tissue.
When Do You Need to See a Doctor?
A fistula could only be the first warning of a more serious problem—for example—an infected—pus-filled area (abscess) or cancer. Reading about the symptoms in the health library is not enough if the symptoms persist. Make sure to see and consult your doctor if you are experiencing any symptoms or signs of a rectovaginal fistula and bring your medical records with you if you have any.
Consult with Arizona Center For Chronic Pelvic Pain—and we’ll identify the cause of the fistula and determine the right treatment plan for you.
Contact our office at 480 599-9682 or email [email protected] to learn more about available treatments.
What is Rectovaginal Fistula?
A rectovaginal fistula is a medical condition characterized by an abnormal connection or passage between the rectum and the vagina, known as the fistula tract. This condition, often referenced in health libraries and by healthcare professionals, can result from various causes, including obstetric trauma during childbirth, tissue damage from radiation therapy, complications from surgeries such as open hysterectomy, and inflammatory bowel diseases like Crohn’s disease and ulcerative colitis. Among the spectrum of genitourinary fistulas, which include vesicovaginal and enterovaginal fistulae, the rectovaginal variant presents with distinctive rectovaginal fistula symptoms. These symptoms may include fecal incontinence, where stool might leak into the vagina, frequent vaginal infections due to the continuous presence of fecal matter in the vaginal area, and the passage of gas from the vagina during a bowel movement. Additionally, patients might notice an offensive odor emanating from the vaginal area, originating from the fistula tract, which can significantly impact their quality of life.
Addressing rectovaginal fistulae requires an in-depth understanding of the condition basics and a thorough diagnostic approach. Advanced practitioners or health care providers typically begin with a physical examination of the pelvic area and may recommend imaging studies like a CT scan to visualize the fistula’s exact location and the extent of the tissue breakdown. In cases where the condition is suspected to be a result of inflammatory diseases like Crohn’s disease, confirming the underlying medical condition is crucial before embarking on treatment. The World Health Organization and other prominent health bodies have highlighted the importance of early diagnosis and intervention. The primary treatment for this ailment is rectovaginal fistula repair, which involves surgical closure of the abnormal connection, ensuring that the healthy tissue surrounding the fistula tract is preserved. In cases like the colovaginal fistula, which involves the colon and the vagina, or the vesicovaginal tract fistulas, which concern the bladder and the vagina, the repair approach might differ. Regardless of the type, timely consultation and intervention by a qualified health care provider are essential to ensure optimal patient outcomes and reduce the risk of complications such as tissue breakdown, infection, and persistent urinary or fecal incontinence.
