Müllerian Duct Anomaly
What Are Mullerian Anomalies?
Mullerian anomalies can affect up to four percent of the female population. The anomaly is considered a ‘hereditary disorder’; this indicates that this complication occurs during fetal development and is present during childbirth. As an embryo forms, the two paired Mullerian ducts will develop into the female genital tract, including the fallopian tube, uterus, cervix, and upper two-thirds of the vagina.
A Mullerian duct anomaly with congenital rectovaginal fistula is a very rare Mullerian abnormality or infection that may generate a gynecological and obstetric infection or complication, such as Dis colon rectum or problem with the rectum, colorectal dis, Crohn’s disease, colovesical fistula, diverticulitis, stool abnormalities, enterovesical fistula, fecal incontinence, inflammatory bowel disease, diverticular disease, which requires a surgery to treat or surgical intervention.
Mullerian abnormality, like rectovaginal fistula, is often associated with renal and axial skeletal abnormalities. Congenital rectovaginal fistula, imperforate anus (malformation of the anal canal which happens during childbirth), hypospadias (childbirth defect in boys), and other anatomical variants of cloacal dysgenesis can also be part of maldevelopment of the Mullerian and mesonephric duct derivatives.
For women, internal reproductive organs such as fallopian tubes, uterus, and upper part of the vagina derive from Mullerian ducts. Mullerian ducts are structures present in the fetus. Those ducts during fetal development undergo multiple changes, including fusion of the left and right sides.
Abnormalities in the formation of the Mullerian ducts lead to anomalies such as the bicornuate uterus, vaginal septum, or vaginal agenesis. Patients born with vaginal agenesis, also called Mayer–Rokitansky–Küster–Hauser syndrome (MRKH), do not have a uterus, cervix, or most of the vagina. Generally, the syndrome is discovered around the time of menarche because patients, despite normal sexual development, do not have a menstrual period.
Surgical treatments are available to create a functional vagina. One of the most successful procedures in patients with MRKH syndrome is the minimally invasive Vecchietti procedure. A fully functional vagina comparable to a normal vagina can be reconstructed using this procedure. It requires only three small laparoscopic incisions, which are cosmetically very desirable for a young patient.
Mullerian Defect On Female Reproductive Tract (Rectovaginal Fistula)
Just like the bladder, rectum, rectovaginal septum, and other organs in the body, a woman’s reproductive organs take form when she is still a fetus inside her mother’s uterus. These reproductive organs include the uterus and fallopian tubes, which develop from two ducts known as the müllerian ducts.
During normal development, these two ducts come together. However, there are times when fistula formation occurs. Fistula formation happens when the uterus and fallopian tubes don’t form as they should. These malformations are called Mullerian anomalies that make it difficult or impossible for a woman to get pregnant without getting surgery to treat it.
How Is The Condition Diagnosed?
Mullerian anomalies are commonly identified at the onset of puberty, when an adolescent begins to menstruate or when a young woman fails to get her menstrual period. Rectovaginal fistula may also be diagnosed when a woman experience trouble conceiving or maintaining a pregnancy. Some anomalies are associated with a common cause or symptom. Some of the symptoms that you might feel if you have a rectovaginal fistula are:
- Abdominal or pelvic pain
- Discomfort during sex
- Menstrual abnormalities
- Palpitation
- Stool abnormalities
Mullerian anomaly or infection and a reproductive underlying disease or condition can be diagnosed with imaging technology. Diagnostic testing may include:
- Pelvic ultrasound
- Three-dimensional ultrasound
- Magnetic resonance imaging (MRI)
- Hysterosalpingogram (HSG)
- Laparoscopy hysteroscopy
In most cases, Mullerian anomaly fistulae or fistulae such as vesicovaginal fistula and rectovaginal fistula can be left untreated, particularly when it does not significantly affect reproduction. Mullerian anomalies that prevent menstruation or cause significant pain in the urinary bladder, rectum, anus, and sigmoid colon usually requires surgical treatment or surgical repair. Surgery treatment depends on the extent of the individual fistula or if there is an existing underlying disease.
Can A Female With Mullerian Anomaly (Rectovaginal Fistula) Eventually Become Pregnant And Carry To Term?
Mullerian anomalies fistulae or fistula, specifically rectovaginal fistula, may affect fertility. But, if a woman undergoes treatment, the septated uterus can be corrected, which means getting rectovaginal fistula treatment or surgery (e.g., transvaginal repair) can improve the chances of having a successful pregnancy.
Women with a congenital reproductive anomaly, specifically rectovaginal fistula, who have not been able to complete pregnancy within six months of trying should visit a fertility specialist to get an examination or diagnosis of the fistula tract and surgery treatment. Arizona Center for Chronic Pelvic Pain (AZCCPP) has a fertility specialist with a magnificent reproductive surgical technique.
Surgery can repair the defect and eliminate discomfort in the rectum, anus, and bladder during menses or sexual relations, improving fertility and pregnancy outcomes. Arizona Center for Chronic Pelvic Pain’s (AZCCPP) reproductive surgeons is experienced in caring for adolescents and women with Mullerian anomalies. Our physicians are experts in performing surgery for rectovaginal fistula treatment.
ManagingPatients With Mullerian Anomalies
Managing patients with Mullerian anomalies doesn’t only focus on surgery or rectum and rectovaginal fist repair, such as anastomosis. Rather it also includes psychosocial counseling and a diagnosis of the symptoms of the fistula.
Psychosocial Counseling And Support
All patients with Mullerian anomalies should be offered counseling and encouraged to go and connect with peer support groups. Mullerian anomalies don’t only affect the patient’s bladder or rectum or make them abnormal. Fistulae, such as rectovaginal fistula, also have a psychological effect.
Most patients with rectovaginal fistula don’t only experience an abscess. Patients may also experience anxiety and depression that surgery can’t treat. They might even question their female identity and grieve their infertility. The symptoms of a fistula are not easy. Sometimes, surgery is not enough for a patient with a fistula to get better.
The best predictor of good emotional outcomes after their fistula diagnosis is a good relationship between the patient and their loved ones and the ability to share sentiments with family and friends.
Fertility
Patients with an abscess or fistula should be addressed with their future options for having children. An abscess or fistula can’t stop anyone who wants to be a parent. Adoption and gestational surrogacy are some of the patients with abscesses or fistula options to have children.
Assisted reproductive techniques with the help of a gestational carrier (surrogate) are thriving for women with fistula. Understanding the future fertility options of patients with fistula allows them to understand their potential for becoming parents, which may help them cope with the diagnosis, implications, and surgery.
Assessing The Patient’s Readiness
Nonsurgical or surgical treatment on the rectum, vagina, or other organs should wait until the patient is physically and emotionally ready to proceed with treatment. There are multiple risks of failure of nonsurgical or surgical treatment (e.g., interpersonal conflict, parental misunderstanding of diagnosis, poor motivation, unstable relationships, sociocultural factors, and mental health issues).
Cognitive issues that affect treatment adherence may include the following:
- Limited comprehension of the diagnosis and anatomy
- Young age
- Underlying learning disability
- Inadequate knowledge of the treatment process
- Lack of privacy and limited ability to travel to a clinic for close follow-up
Vaginal Elongation
Primary vaginal elongation repair by dilation is the appropriate first-line technique in most patients because it is safer, cost-effective, and patient-controlled than surgery. Primary vaginal elongation repair is a successful technique. When well-counseled and emotionally prepared, primary vaginal elongation repair lets 90 to 96% of the patients will be able to achieve anatomic and functional success.
General Gynecologic Care
Routine gynecology questions, which include asking for a patient’s personal information, are necessary, such as asking the date of the last menstrual period. The patient should also be asked about any vaginal bleeding, discharge, pelvic pain, abnormalities with their stool, pain in their rectum, as well as irritation with their skin.
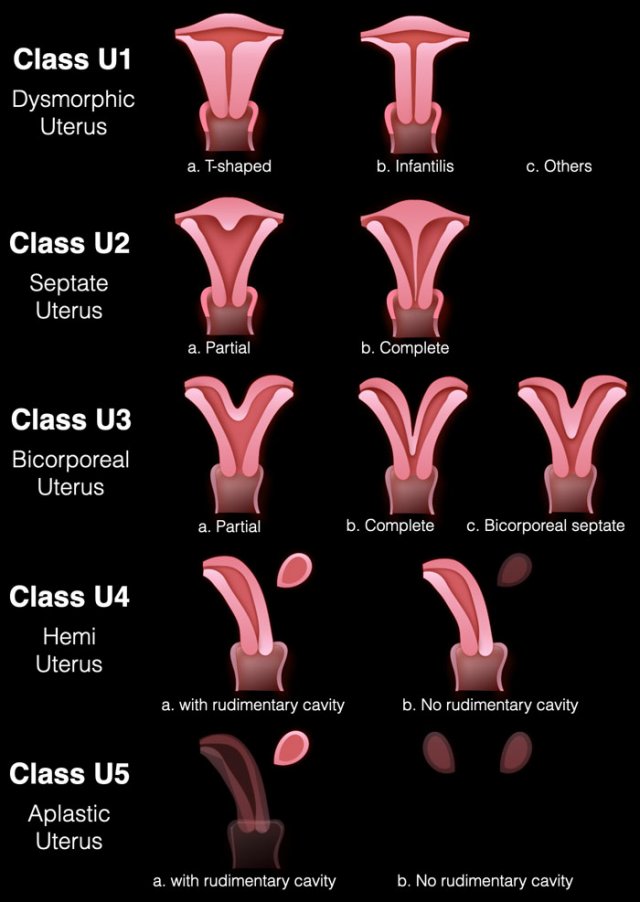
What Types of Müllerian Anomalies Exist?
There are several different forms of müllerian anomalies ranging from the absence of a to the formation of a half or a double to a divided by a septum. All types affect the reproductive tract to varying degrees. They include:
& hypoplasia: Mayer-Rokitansky-Kuster-Hauser syndrome is the most common. All or part of the müllerian tract fails to form or is extremely underdeveloped.
(UU): When one is underdeveloped or fails to develop, a banana-shaped half- is formed. A missing kidney or other kidney problems accompany this asymmetric more than they do other müllerian anomalies. This is a rare condition. (UD): Commonly referred to as a ‘double .’ There may be complete duplication of the vagina, cervix, and , and the two halves may be divided by a ligament of connective tissue. UD has the best outcomes of all the MAs. (BU): This is the most common form of müllerian . Described as a womb with two horns. The womb is not pear-shaped; instead, it is shaped like a heart, with a deep indentation at the top. This means that the baby has less space to grow than in a normally shaped womb.
: Occurs when the inside of the is divided by a wall or the septum. The septum may extend only part way into the or it may reach as far as the cervix.
DES-related : A T-shaped , dilated horns, and malformed cervix and upper vagina may characterize this . A T-shaped is sometimes caused by maternal ingestion of DES, although sometimes the cause is unknown.
(AU): The fundus of the may be indented slightly both inside and outside. The shape is so slight that it is considered a variation of normal.
What is the most common ?
(BU): This is the most common form of müllerian .
What causes abnormalities?
A may be a or may arise due to an infection or prior surgery.
Some of the most commonly seen are:
Correct Diagnosis
The most important steps in effectively treating Mullerian anomalies are a correct diagnosis of the underlying condition, correct evaluation for associated congenital anomalies, and psychosocial counseling. The treatment for Mullerian anomalies doesn’t only focus on treating the patient’s organs, such as the bladder, rectum, anus, etc. Counseling is also very important in addition to treatment or intervention to address the functional effects of genital anomalies.
Expert Care At Arizona Center for Chronic Pelvic Pain (AZCCPP)
We have top-rated pediatric and adolescent gynecologists (for children up to age 18) who are the best ones in Arizona and specialize in diagnosing and treating the most complex Mullerian anomalies in children and adolescent females and males, whether they’re pregnancy-related or otherwise.
We also have skilled reproductive endocrinologists (for adults over age 18) who have expertise in Mullerian anomalies in adults. At AZCCPP, we understand the importance of having a support system when it comes to considering treatment choices for Mullerian anomalies. The start of puberty and family planning are important times, and our team of experts is always here to speak to all of our patients about their options and what they can expect from our treatment plans.
If you or anyone you know has Mayer–Rokitansky–Küster–Hauser syndrome (MRKH) contact our office at 480 599-9682 or email [email protected] to learn about available treatments.
Müllerian duct anomalies
Müllerian duct anomalies, often referred to within the realm of reproductive medicine, are a group of congenital anomalies that result from the abnormal formation, fusion, or resorption of the paramesonephric ducts during embryonic development. These ducts, commonly known as Müllerian ducts, are essential precursors in female fetal development, laying the foundation for the majority of the structures within the female reproductive system. When there’s a disruption in their typical development process, it can lead to various uterine and vaginal anomalies that can have significant implications on human reproduction. For instance, a uterine septum, one of the most common müllerian duct anomalies, refers to a malformation where a wall of tissue divides the uterine cavity either partially or wholly. Other known malformations include the uterine didelphys, where a woman has two separate uterine horns and possibly a didelphys uterus, and cervical agenesis, which refers to the absence of the cervix.
The consequences of müllerian duct anomalies can range from menstrual complications to challenges in achieving and maintaining a pregnancy. For example, an obstructive anomaly, such as a transverse vaginal septum or an obstructed hemivagina, can lead to the accumulation of menstrual blood, causing pain and complications if not diagnosed and treated, often through surgical intervention or vaginal dilation. Women with these conditions might experience issues related to pregnancy loss or preterm birth. Longitudinal vaginal septum and uterine malformations like the uterine didelphys can also present challenges during childbirth. Furthermore, there’s an established association between müllerian anomalies and renal anomalies, making it crucial to evaluate renal anatomy in individuals diagnosed with a müllerian duct anomaly. As the field of reproductive medicine continues to advance, there’s an increasing understanding and ability to address and manage these congenital abnormalities, offering women with müllerian duct abnormalities more comprehensive care and improved reproductive outcomes.
