Interstitial Cystitis (IC), alternatively known as Bladder Pain Syndrome (BPS), is a chronic, often debilitating condition characterized by recurring pain or discomfort in the bladder and the surrounding pelvic region.
Recent research shows a link between IC/BPS and Pudendal Neuralgia (PN), a painful nerve inflammation. This article shows you that you can be free from bladder pain with the right Interstitial Cystitis management and lifestyle.
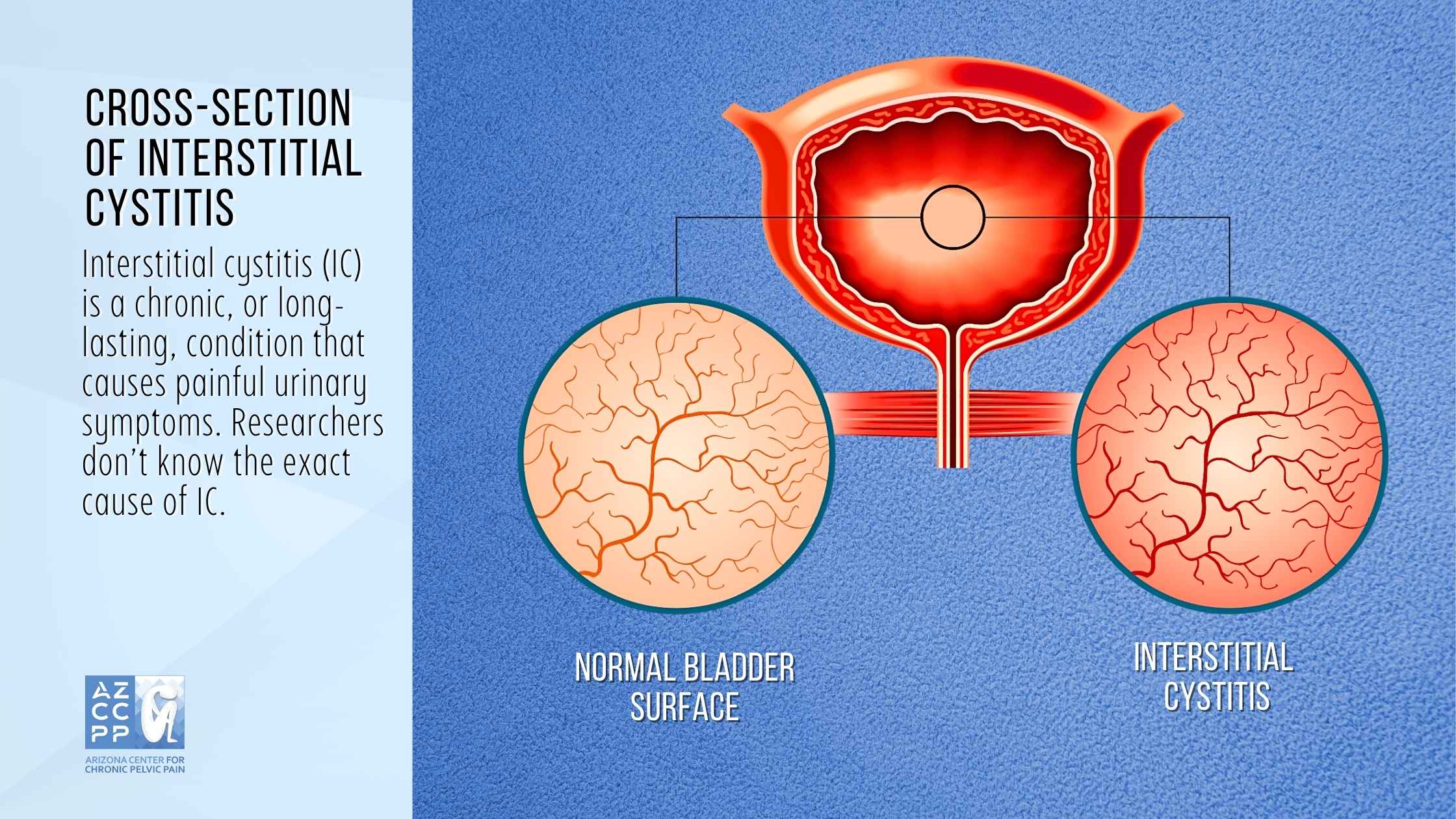
What is Interstitial Cystitis?
1. Symptoms of Interstitial Cystitis
Interstitial Cystitis can cause a variety of symptoms, including:
- Pelvic Pain or Discomfort: According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), IC is the most common symptom of IC, and it can be felt in the lower abdomen, pelvis, or vagina. The pain can be burning, stabbing, or persistent, and it can be worse at night or after sexual intercourse.
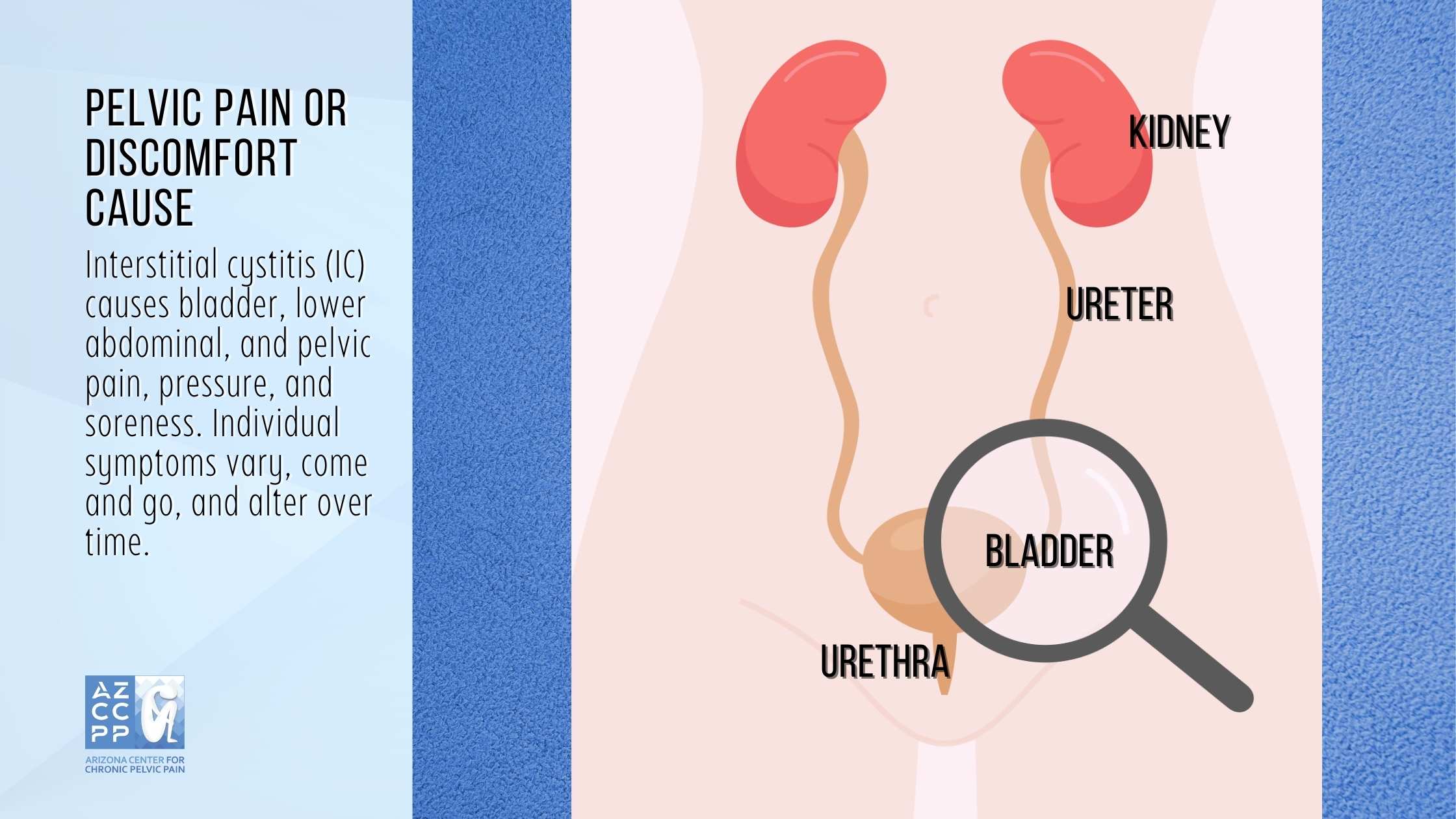
- Urinary Urgency: This is a sudden, strong need to urinate that cannot be ignored. People with IC may feel like they need to urinate all the time, even when their bladder is not full.
- Frequent Urination: People with IC may urinate up to 60 times a day, even at night.
- Painful Urination: This is pain that occurs during urination. The pain can be burning, stinging, or sharp.
- Pelvic Tenderness: This is a feeling of pressure or fullness in the pelvis.
- Pain During Sex: This can be a pain in the penis, vulva, or vagina.
- Other symptoms of IC: Fatigue, depression, anxiety, difficulty sleeping, and changes in bowel habits
2. Causes of Interstitial Cystitis
The exact cause of IC is unknown. However, there are several theories about what may cause the condition, including:
- Defect in the bladder lining: The bladder lining is normally a protective barrier that prevents harmful substances from entering the bladder wall. In people with IC, this lining may be defective, allowing irritants to enter the bladder wall and cause inflammation.
- Nerve problems: Some people with IC have abnormalities in the nerves that control the bladder. These abnormalities may cause the bladder to send pain signals to the brain, even when the bladder is not full.
- Autoimmune disorders: IC may be linked to autoimmune disorders, which are conditions in which the body’s immune system attacks healthy tissues.
- Allergies: Some people with IC have allergies to certain foods or other substances, which may trigger IC symptoms.
- Infection: In some cases, IC may be caused by an infection. However, this is not always the case.
3. Diagnosis of Interstitial Cystitis
There is no single test to diagnose IC. The diagnosis is usually made based on the patient’s symptoms and a physical examination. In some cases, the doctor may perform a cystoscopy, which is a procedure that allows the doctor to look inside the bladder.
The severity of IC symptoms can vary from person to person. Some people may have mild symptoms that do not interfere with their daily lives, while others may have severe symptoms that make it difficult to work, sleep, and enjoy social activities.
4. Treatment of Interstitial Cystitis
There is no cure for IC, but there are treatments that can help manage the symptoms. Treatment options include:
- Lifestyle changes: Some lifestyle changes, such as avoiding caffeine, alcohol, and spicy foods, can help reduce IC symptoms.
- Medications: Several medications can be used to treat IC. These medications can help reduce bladder pain, urgency, and frequency.
- Physical therapy: Physical therapy can help to strengthen the pelvic muscles and improve bladder control.
- Nerve stimulation: Nerve stimulation is a procedure that uses electrical currents to stimulate the nerves that control the bladder. This can help to reduce bladder pain and urgency.
- Bladder instillations: Bladder instillations involve putting medication directly into the bladder. This can help to reduce bladder pain and inflammation.
The most critical components of diagnosing interstitial cystitis are a detailed examination of symptoms and a physical exam in a doctor’s office. A healthcare expert will inquire if you have a history of health issues associated with IC.
5. What Triggers Interstitial Cystitis Symptoms?
Interstitial Cystitis symptoms can be exacerbated by a variety of factors known as symptom triggers. These triggers can vary from person to person, and identifying them can play a crucial role in managing IC symptoms effectively.
- Stress: One common trigger for IC symptoms is stress. When the body experiences stress, it releases hormones that can heighten bladder sensitivity and increase pain perception. Additionally, anxiety can also aggravate IC symptoms, as the body’s fight-or-flight response can lead to increased bladder muscle contractions.
- Menstruation: A woman’s period can also be a trigger for IC symptoms. Hormonal fluctuations during menstruation can irritate the bladder lining, leading to increased urgency, frequency, and pain during urination.
- Sexual Intercourse: Having sexual intercourse can also aggravate IC symptoms. The friction and pressure of sexual activity can irritate the bladder lining and trigger pain, especially for women with IC.
- Food: Certain foods and drinks can also act as symptom triggers. Caffeine, alcohol, spicy foods, and acidic foods can all irritate the bladder lining and worsen IC symptoms.
- Smoking: This is another potential trigger for IC symptoms. The chemicals in cigarettes can irritate the bladder lining and contribute to inflammation.
- Medication: Certain medications, such as antihistamines and decongestants, can also trigger IC symptoms. These medications can dry out the bladder lining, making it more susceptible to irritation.
By identifying and avoiding symptom triggers, individuals with IC can actively manage their symptoms and improve their overall quality of life.
Interstitial Cystitis Management
Interstitial Cystitis can significantly impact a person’s quality of life, affecting their social, work, and emotional well-being. IC management is crucial to reducing symptoms, improving bladder function, and enhancing overall health.
1. Interstitial Cystitis Diet
Diet can be crucial in managing IC symptoms, as certain foods and drinks might aggravate the bladder and increase discomfort. Managing Interstitial Cystitis (IC) often involves making dietary modifications to reduce symptoms and improve overall well-being. Here are some key dietary considerations to keep in mind:
-
Avoid Trigger Foods
Certain foods can exacerbate IC symptoms, so it’s important to identify and eliminate personal triggers. Common trigger foods include:
➢ Citrus Fruits: Citrus fruits, such as oranges, grapefruits, and lemons, contain high levels of vitamin C and citric acid, which can irritate the bladder lining.
➢ Spicy Foods: Spicy foods, such as chili peppers, hot sauces, and curries, contain capsaicin, a compound that can aggravate IC symptoms.
➢ Caffeinated Beverages: Caffeine, found in coffee, tea, and soda, can increase bladder urgency and frequency.
-
Embrace a Balanced Diet
A balanced and nutritious diet can help support overall health and reduce IC symptoms. Consider incorporating these dietary elements:
➢ Alkaline Foods: Alkaline foods, such as vegetables and non-citrus fruits, tend to be less irritating to the bladder lining. Good options include leafy greens, cucumbers, carrots, bananas, and melons.
➢ Adequate Water Intake: Drinking plenty of water throughout the day helps dilute urine and prevent concentrated urine, which can irritate the bladder. Aim for at least eight glasses of water daily.
➢ Fiber-Rich Foods: Fiber-rich foods, such as whole grains, fruits, and vegetables, can help prevent constipation, which can aggravate IC symptoms. Adequate fiber intake promotes regular bowel movements and reduces strain on the bladder.
-
Personalized Diet Plans
Developing a personalized diet plan tailored to individual needs and triggers is crucial for effective IC management. Keeping a food diary can help identify personal triggers and guide the development of an individualized, balanced diet.
By following these dietary considerations and working closely with a healthcare professional or registered dietitian, individuals with IC can take proactive steps to manage their symptoms and improve their overall quality of life.
2. Interstitial Cystitis Self-Care
Interstitial Cystitis (IC), a chronic condition characterized by bladder pain, urgency, and frequency, can significantly impact one’s quality of life. Self-care is pivotal in managing IC symptoms and empowering individuals to reclaim control over their well-being.

Here are some effective self-care strategies to consider:
-
Stress Management
Stress, a common trigger for IC symptoms, can be effectively managed through various relaxation techniques. Meditation, deep breathing exercises, and yoga are excellent practices for reducing stress levels and potentially alleviating IC symptoms. Incorporating these techniques into a daily routine can promote a sense of calm and improve overall well-being.
-
Pelvic Floor Physical Therapy
Pelvic floor muscles play a crucial role in bladder control. Strengthening and relaxing these muscles through pelvic floor physical therapy can alleviate pelvic pain and discomfort associated with IC. Working with a trained physical therapist can provide personalized exercises and stretches tailored to individual needs, helping to improve bladder function and reduce symptom severity.
-
Bladder Training
Retraining the bladder is an effective self-care strategy for managing IC. Bladder training involves gradually increasing the time between urinations, helping to reduce bladder overactivity and urgency. This process involves creating a bladder diary to track urination patterns and gradually increasing the intervals between bathroom visits. By gradually extending the time between urinations, the bladder learns to hold more urine, reducing the frequency of bathroom trips and alleviating IC symptoms.
-
Heat or Cold Therapy
Applying heat or cold packs to the pelvic area can temporarily relieve IC pain and discomfort. Heat therapy can help relax tense muscles and promote blood flow, while cold therapy can reduce inflammation and numb pain sensations. Experimenting with both heat and cold therapy can help identify the most effective approach for individual relief.
In addition to these specific self-care strategies, adopting a healthy lifestyle can further support IC management. Maintaining a balanced diet, avoiding trigger foods, staying hydrated, and getting regular exercise can all contribute to overall well-being and symptom reduction. By incorporating these self-care practices into their daily lives, individuals with IC can take an active role in managing their condition and improving their quality of life.
-
Physical Therapy
Physical therapy can treat IC. In fact, it is often recommended as a first-line treatment. Physical therapy can help reduce pain, improve bladder function, and increase quality of life.

Physical therapy can be very effective for IC. In one study, 80% of people with IC who received physical therapy reported a significant improvement in their symptoms. Here are some of the benefits of physical therapy for IC:
- Reduced pain
- Improved bladder function
- Increased quality of life
- Decreased need for medication
If you are considering physical therapy for IC, it is important to find a therapist who is experienced in treating this condition. As one of Arizona’s best physical therapy providers, AZCCPP includes physical therapy in our pelvic pain treatments.
Chronic pelvic pain and other pelvic diseases are difficult, requiring multimodal therapy. We combine your information, clinical knowledge, and medical evaluation with Dr. Hibner and physical therapy evaluation with Tiffany to improve diagnostic and treatment quality and speed, giving you a better overall picture to make the most individualized care decisions.
Interstitial Cystitis Life Expectancy
Interstitial Cystitis does not directly impact life expectancy. However, the chronic pain and discomfort associated with the condition can significantly impair the quality of life. Proper management of symptoms, maintaining a healthy lifestyle, and regular medical check-ups can help individuals with IC lead relatively normal and productive lives.
Recent Advancements in Interstitial Cystitis Management and Research
The ongoing pursuit of effective IC management continues to fuel active research and development in this area. Recent advancements have shed light on the complex mechanisms underlying IC and expanded the therapeutic landscape with promising new treatment modalities.
Deeper Understanding of IC Pathophysiology
Researchers are delving deeper into the intricate mechanisms contributing to IC, uncovering new insights into its pathophysiology. Studies have identified potential roles for neurogenic inflammation, autoimmunity, and abnormalities in the development of the bladder’s protective lining (epithelium) of IC. These findings offer valuable targets for the development of novel treatment approaches.
Emerging Treatment Modalities
The IC treatment landscape is evolving, with several promising new therapeutic interventions under investigation. These include:
-
Intravesical dimethyl sulfoxide (DMSO): DMSO, a naturally occurring compound, has demonstrated efficacy in reducing IC symptoms in clinical trials.
-
Glycosaminoglycan replacement therapy: This approach aims to restore the integrity of the bladder epithelium by replacing lost glycosaminoglycans, which are essential components of the bladder’s protective layer.
-
Nerve modulation: Neuromodulation techniques, such as sacral neuromodulation and sacral ganglion stimulation, are being explored for their potential to alleviate IC pain.
These emerging treatment options offer hope for individuals with IC, providing avenues for personalized and effective symptom management.
Personalized Medicine Approach
The recognition of IC heterogeneity has led to a growing emphasis on personalized medicine, tailoring treatment strategies to individual patient characteristics and needs. This approach involves identifying specific biomarkers and genetic factors that may predict treatment response, enabling more targeted and effective interventions.
Future Directions
Research efforts continue to focus on uncovering the underlying causes of IC and developing more effective and personalized treatment options. The identification of biomarkers, the exploration of novel therapeutic approaches, and the advancement of personalized medicine hold great promise for improving the lives of individuals affected by IC.
Read More About Pudendal Neuralgia Here!
Conclusion
Interstitial Cystitis is a chronic and, at times, profoundly debilitating condition, but through a comprehensive understanding of the condition and strategic lifestyle adjustments, individuals can navigate the challenges it poses.
Adapting one’s diet, embracing self-care practices, and maintaining regular medical checkups are critical steps in managing IC symptoms effectively, improving daily functioning, and maintaining a high quality of life. While the journey with IC can be strenuous, embracing a proactive and informed approach can significantly alleviate the burden and help foster resilience and well-being.
Contact Us for Pudendal Neuralgia Treatment Now!
If you’re experiencing symptoms of Pudendal Neuralgia, don’t delay seeking medical attention. Contact the Arizona Center for Chronic Pelvic Pain for expert diagnosis and personalized treatment. Our experienced team specializes in managing pelvic pain conditions and can provide the care you need to feel better. Call us at (480) 599-9682 or email [email protected] to schedule an appointment.
AZCCPP offers comprehensive evaluation, personalized treatment plans, and compassionate care to help you find relief. Contact us today at (480) 599-9682 or [email protected] to schedule an appointment. You may also check out AZCCPP on YouTube for more questions that need answers with Dr. Michael Hibner.
By understanding the symptoms, causes, diagnosis, and treatment options for Pudendal Neuralgia, you can take proactive steps to manage this condition effectively and regain your quality of life.