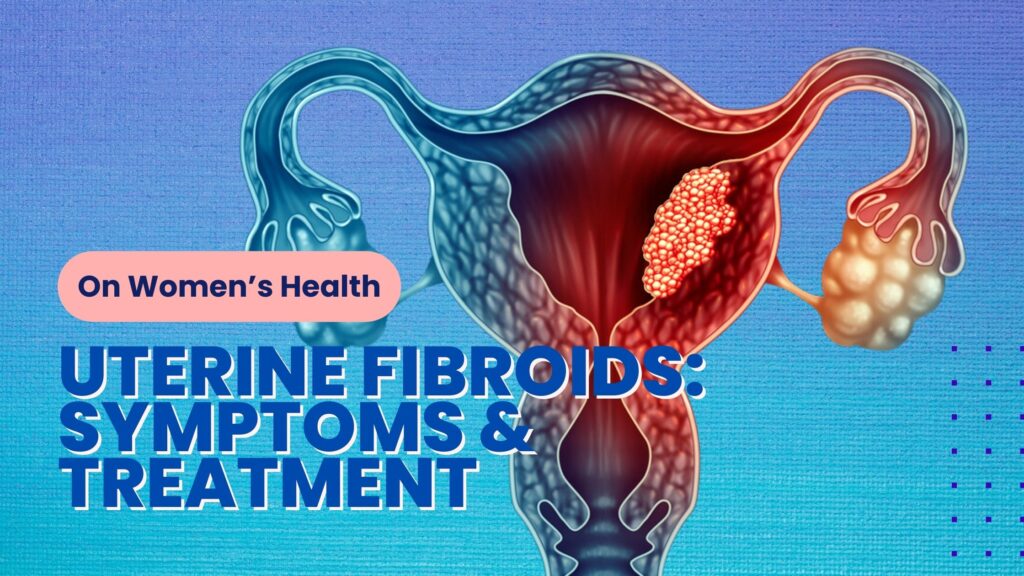
Uterine fibroids, also known as leiomyomas or myomas, are benign tumors that develop within the muscular wall of the uterus. These growths are incredibly common, affecting many women, especially during their reproductive years. While they are typically not cancerous, fibroids can cause a range of symptoms and potential complications.
Fibroids can vary widely in both size and quantity. You may have just one fibroid or multiple. Some are so small they can’t be detected without imaging, while others grow to the size of a grapefruit or even larger. When fibroids grow significantly, they can alter the shape of the uterus, both inside and out. In rare cases, they expand enough to fill the entire pelvic or abdominal area, giving the appearance of pregnancy.
Fibroids are common, with many people experiencing them at some point in their lives. Often, they don’t cause symptoms and may only be discovered incidentally during a pelvic exam or an ultrasound done for pregnancy or other reasons.
Between 2011 and 2022, a total of 16,046 new cases of uterine fibroids were identified among female active component service members in the U.S. Armed Forces, resulting in an incidence rate of 63.5 cases per 10,000 person-years. The highest incidence rates were observed among servicewomen aged 40 years and older, non-Hispanic women of color, and those serving in the Army.
Over this period, while uterine fibroid-related medical encounters and the number of individuals affected increased, the number of hospital bed days decreased from 699 days in 2011 to 625 days in 2022. This decline in hospital bed days may be attributed to early diagnoses and the availability of minimally invasive treatments.
Understanding Uterine Fibroids: What Are They and Why Do They Occur?
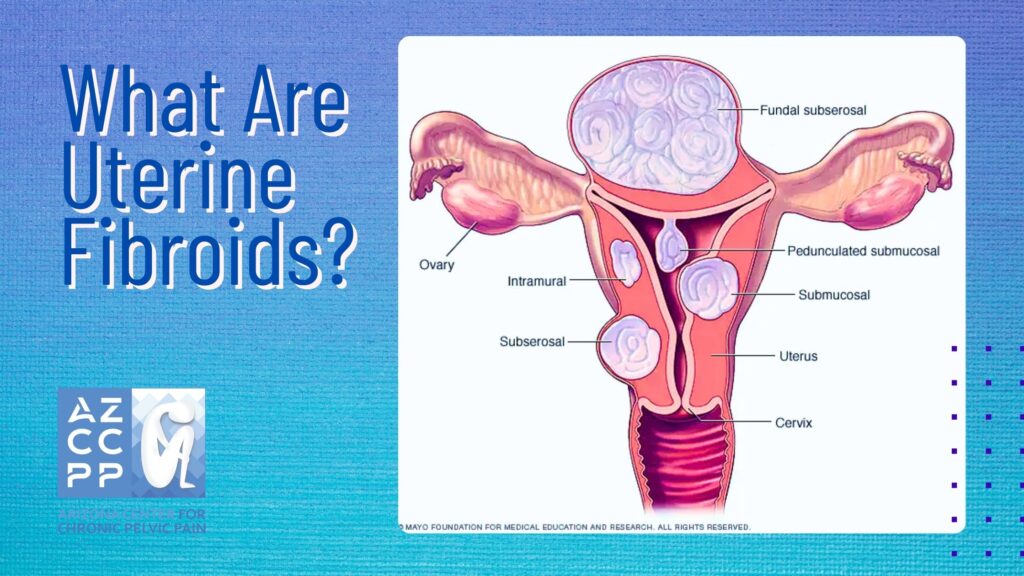
Uterine fibroids, also known as leiomyomas, are benign growths composed of smooth muscle cells and fibrous connective tissue that develop within or on the uterus. Their sizes can vary significantly; some fibroids are as small as a seed, while others can grow large enough to change the shape and size of the uterus.
The specific cause of fibroids remains unknown; however, studies indicate a strong connection to hormonal activity, particularly the influence of estrogen and progesterone, which help stimulate their growth. These hormones are especially influential during reproductive years, which is why fibroids are more common among women in their 30s to 50s and tend to shrink after menopause when hormone levels decrease.
Genetic factors may also play a role, as women with a family history of fibroids are at a higher risk of developing them. Additional research among military populations has found that demographic factors, such as age and race, also contribute to the prevalence of fibroids, with higher incidences observed in women of color and women over 40.
Recognizing the Symptoms: How Do Fibroids Manifest?
The symptoms of uterine fibroids can vary widely based on factors such as their size, number, and exact location within the uterus. While some individuals may not experience any symptoms, others may encounter a range of physical discomforts and disruptions:
- Heavy Menstrual Bleeding: One of the most common symptoms, heavy menstrual bleeding occurs when fibroids affect the uterine lining, resulting in prolonged or excessive bleeding. This can lead to iron-deficiency anemia, a condition marked by fatigue, weakness, and dizziness due to a reduced red blood cell count.
- Prolonged Periods: Fibroids can disrupt the normal menstrual cycle, causing periods to last longer than usual, sometimes extending beyond seven days. This can be particularly disruptive for daily life and may lead to the need for frequent changes of sanitary products, creating added inconvenience and expense.
- Pelvic Pain and Pressure: Larger fibroids, or those located near the outer wall of the uterus, can exert pressure on surrounding organs, resulting in a feeling of fullness or bloating in the abdomen. Particularly if the fibroid presses on nerves or sensitive tissue, this pressure can cause varying degrees of pain, from mild discomfort to severe cramping.
- Painful Intercourse: Fibroids can also interfere with sexual health. When located near the cervix or in other sensitive areas of the uterus, fibroids can make sexual intercourse painful, especially if the fibroid’s location leads to pressure on certain areas during intimacy. This discomfort can affect a woman’s sexual well-being and relationships, making open discussions with healthcare providers important.
- Frequent Urination: Large fibroids may press on the bladder, resulting in frequent urges to urinate or feelings of incomplete bladder emptying. This symptom is particularly bothersome at night, interrupting sleep and potentially leading to daytime fatigue.
- Constipation: When fibroids grow near the rectum, they can create pressure on the bowel, making it difficult to pass stool or causing constipation. This can lead to abdominal pain, bloating, and discomfort, sometimes requiring dietary changes or medications to manage.
- Backache or Leg Pains: In cases where fibroids press on spinal nerves or nerves in the pelvic area, women may experience referred pain in the lower back or even down the legs. This can make physical activities challenging and interfere with overall mobility and comfort.
Diagnosing Uterine Fibroids: Tests and Procedures
If you suspect that you may have uterine fibroids, consulting with a healthcare provider is the first step toward effective management. Your provider will typically begin with a pelvic exam to check for any abnormalities in the size, shape, and feel of the uterus, as fibroids can often cause noticeable changes. Based on the exam, further diagnostic tests may be recommended to confirm the presence of fibroids and to assess their size, number, and specific locations within the uterus. Here are some of the most common diagnostic procedures:
-
Ultrasound
This non-invasive imaging technique uses sound waves to create detailed images of the uterus and fibroids. During a transabdominal ultrasound, a device (transducer) is moved over the abdomen, while in a transvaginal ultrasound, a smaller transducer is inserted into the vagina to get a closer view. Ultrasounds are often the first-line imaging choice as they effectively reveal fibroid size, shape, and location.
-
MRI (Magnetic Resonance Imaging)
MRI provides a more detailed look at fibroids than ultrasound and is particularly useful for identifying the number, size, and exact positioning of fibroids, especially in cases where fibroids are deep within the uterine wall or if surgery is being considered. MRI can help distinguish fibroids from other pelvic conditions and is often used when precise mapping is needed for treatment planning.
-
Hysteroscopy
This minimally invasive procedure involves inserting a thin, lighted telescope (hysteroscope) through the vagina and cervix into the uterus to view the uterine cavity. Hysteroscopy allows the provider to directly visualize and evaluate fibroids located inside the uterine cavity (submucosal fibroids), which can be a source of heavy menstrual bleeding. It also enables the removal of smaller fibroids during the procedure if necessary.
-
Endometrial Biopsy
In cases where heavy bleeding is a symptom, an endometrial biopsy may be performed to take a small tissue sample from the uterine lining. This test helps rule out other causes of abnormal bleeding, such as endometrial hyperplasia or cancer. The sample is analyzed in a laboratory to provide additional insights into the uterine environment, although the biopsy itself does not diagnose fibroids.
-
Sonohysterography
Sometimes used in conjunction with ultrasound, this procedure involves inserting a sterile saline solution into the uterus via a thin tube placed through the cervix. The saline expands the uterine cavity, allowing clearer ultrasound images, particularly of fibroids or other abnormalities inside the uterus. Sonohysterography is beneficial for identifying smaller fibroids that may otherwise go undetected in a standard ultrasound.
Each of these diagnostic tools provides valuable insights, allowing healthcare providers to develop a personalized treatment plan that addresses the unique nature of each fibroid case. Early and accurate diagnosis is essential to guide treatment decisions and optimize outcomes.
Treatment Options: Managing Uterine Fibroids
The appropriate treatment for uterine fibroids depends on various factors, including the severity of symptoms, the size and number of fibroids, and your desire for future fertility. Treatment options include:
-
Watchful Waiting
If fibroids are small and asymptomatic, your doctor may recommend monitoring them without immediate intervention.
-
Medications
Hormonal medications like gonadotropin-releasing hormone (GnRH) agonists can shrink fibroids, but they are often used temporarily due to potential side effects. Other medications may be prescribed to manage pain or heavy bleeding.
-
Minimal Invasive Procedures
-
- Uterine Fibroid Embolization (UFE) blocks blood flow to the fibroids, causing them to shrink.
- Myolysis: This involves using heat or cold to destroy fibroid tissue.
- Radiofrequency Ablation: High-energy radio waves are used to shrink fibroids.
-
Surgical Procedures
-
- Myomectomy: This surgery removes fibroids while preserving the uterus, making it a suitable option for women who wish to maintain their fertility.
- Hysterectomy: This involves the removal of the entire uterus and is often considered a definitive treatment for fibroids.
Living with Uterine Fibroids: Managing Symptoms and Maintaining Quality of Life
Managing uterine fibroids is not only about addressing physical symptoms but also involves lifestyle adjustments and emotional support.
Here are key strategies:
- Pain Management: Over-the-counter NSAIDs, like ibuprofen, are often recommended for managing pain. For cases that don’t respond to NSAIDs, hormonal treatments (such as birth control pills, GnRH agonists, or selective progesterone receptor modulators) can help reduce the size of fibroids, decreasing pain and other symptoms.Some patients may also benefit from pain management clinics that offer multi-disciplinary approaches, including physical therapy and mental health support [National Institute of Child Health and Human Development].
- Iron Supplements: Heavy menstrual bleeding from fibroids can cause iron-deficiency anemia. Healthcare providers often recommend daily iron supplements or iron-rich foods to help manage anemia symptoms, such as fatigue and weakness.In severe cases, iron infusions or even blood transfusions might be needed. Studies show that managing anemia effectively improves the quality of life, making this step crucial [American Society of Hematology].
- Dietary Changes: A well-balanced diet rich in iron, fiber, and antioxidants may help manage fibroid symptoms. Some studies suggest that a diet high in green vegetables, fruits, and dairy products could reduce fibroid risk, whereas excessive red meat and processed foods might promote fibroid growth.Avoiding high-estrogen foods, like soy, may also benefit those whose fibroids are hormonally sensitive [Harvard T.H. Chan School of Public Health].
- Stress Management: Chronic stress can aggravate fibroid symptoms and negatively impact overall health. Engaging in stress-relieving practices like yoga, mindfulness meditation, and breathing exercises can help reduce pain and improve emotional resilience.Research indicates that physical activities such as walking and swimming not only alleviate stress but also promote hormonal balance, potentially reducing fibroid size and severity [National Center for Complementary and Integrative Health].
When to Seek Medical Attention: Recognizing Red Flags
Although uterine fibroids are typically non-cancerous, certain symptoms necessitate immediate medical evaluation. Recognizing and addressing these symptoms early can prevent serious complications:
- Sudden, Severe Pelvic Pain: Intense pelvic pain might indicate fibroid degeneration (a condition where the blood supply to a fibroid is cut off, causing it to die) or torsion, especially if the fibroid is pedunculated (attached to the uterus by a stem). Sharp pain is also a red flag for other potential conditions, such as ovarian cysts or ectopic pregnancy, that require prompt treatment.
- Excessive Bleeding: If menstrual bleeding soaks through pads or tampons hourly or lasts more than seven days, immediate medical care is advised. Untreated heavy bleeding can lead to severe anemia, heart palpitations, and shortness of breath, potentially requiring hospitalization.
- Fever: Particularly following recent fibroid-related surgery, a fever along with pelvic pain or unusual vaginal discharge may indicate a rare but serious infection. Infections can rapidly spread in the reproductive system, causing conditions like pelvic inflammatory disease, so prompt medical intervention is essential.
- Rapidly Growing Fibroid: Rapid growth of a fibroid or a new onset of symptoms in postmenopausal women can sometimes suggest a rare cancerous change called leiomyosarcoma. While this is uncommon, any concerning changes should be evaluated by a gynecologist for further testing, including imaging or a biopsy [Johns Hopkins Medicine].
Uterine Fibroids: A Common Concern, Not a Life Sentence
Uterine fibroids are one of the most prevalent gynecologic conditions, affecting up to 80% of women by age 50, with higher rates observed among African American women. While fibroids can cause significant symptoms, most women can manage them effectively with proper treatment and lifestyle adaptations.
Staying informed, advocating for one’s health, and collaborating with healthcare providers are all important steps to maintain a good quality of life. Resources like the Fibroid Foundation and the Office on Women’s Health offer information and support for individuals navigating this condition [Fibroid Foundation; Office on Women’s Health].
The Future of Fibroid Treatment: Emerging Therapies

New advancements in fibroid treatment provide more options beyond traditional surgery, offering less invasive, effective alternatives:
- Focused Ultrasound Surgery (FUS): This non-invasive outpatient procedure uses MRI-guided high-intensity ultrasound waves to heat and destroy targeted fibroid tissue. FUS is particularly effective for symptomatic fibroids and is associated with quick recovery times. Patients treated with FUS report significant symptom relief without the need for incisions or general anesthesia [National Institutes of Health].
- Myometrial Ablation: This minimally invasive treatment uses radiofrequency or microwave energy to ablate, or destroy, fibroid tissue. Unlike a hysterectomy, it preserves the uterus, which is especially important for women considering future pregnancies. Recovery time is shorter than traditional surgery, and this procedure is often performed as an outpatient treatment [Society of Interventional Radiology].
- Drug Therapies: New medications are under development to target hormonal and growth factors contributing to fibroid growth. For instance, selective progesterone receptor modulators (SPRMs) and gonadotropin-releasing hormone (GnRH) antagonists have shown promise in reducing fibroid size and controlling heavy bleeding. Additionally, newer therapies aim to address specific fibroid-related symptoms, such as Elagolix, which has recently been approved for fibroid treatment. This non-hormonal therapy offers a new approach for those who cannot tolerate or wish to avoid hormonal treatments [FDA].
- Gene Therapy and Stem Cell Research: Ongoing studies in gene therapy and stem cell research hold future potential for fibroid treatment by identifying genetic markers associated with fibroid growth. In time, these approaches may lead to personalized treatments that target the underlying causes of fibroids, rather than just managing symptoms.
- Embolization Techniques: Uterine artery embolization (UAE) is another minimally invasive procedure that involves injecting small particles into the uterine arteries to block blood flow to the fibroids, causing them to shrink. UAE has shown promising results in significantly reducing symptoms and is an option for women who want to preserve their uterus but wish to avoid surgery [American College of Radiology].
With these emerging therapies, fibroid treatment is moving toward less invasive, patient-centered care that emphasizes symptom relief and fertility preservation. As research continues, the future holds promising options for women affected by this common condition.
Conclusion
Uterine fibroids can pose significant challenges, impacting various aspects of daily life. However, with recent advancements in diagnosis and treatment, there are now more ways than ever for women to manage fibroids effectively and improve their quality of life. By educating yourself about fibroid symptoms, seeking timely and appropriate medical care, and exploring personalized treatment options, you can regain control over your health and well-being.
At the Arizona Center for Chronic Pelvic Pain, we are dedicated to providing compassionate, comprehensive care tailored to meet the unique needs of each woman facing fibroid-related concerns. Our experienced team of specialists understands the complexities of pelvic health and is committed to guiding you through every step of your journey—from diagnosis to finding the treatment plan that best aligns with your lifestyle and health goals.
READ MORE: Comprehensive Guide of Symptoms & Treatments for Vulvodynia
Contact Us for Uterine Fibroids Treatment for Women

Don’t let uterine fibroids disrupt your life. Connect with us to discuss your symptoms, ask questions, and receive expert support for managing your health. Schedule a personalized consultation today by calling (480) 599-9682 or emailing us at [email protected]. Together, we can take proactive steps toward relief, clarity, and a healthier future. Visit Arizona Center for Chronic Pelvic Pain to learn more about our services and how we can support your journey.
Check out AZCCPP on YouTube for more questions that need answers with Dr. Michael Hibner.