Endometriosis is a condition in which the tissue that normally is present inside the cavity of the uterus, called endometrium, starts growing on the pelvic walls, ovaries, fallopian tubes, bladder, bowels and occasionally pelvic nerves. Despite extensive research it is unclear how patients get endometriosis. There are multiple theories attempting to explain the etiology of this disease. One of the most popular, called Sampson’s theory, states that endometrial cells travel to the pelvis through the fallopian tubes with menstrual blood. Those cells then implant on the pelvic organs, ovaries, fallopian tubes, bowel, bladder and pelvic side walls. The second theory called Myers theory of coelomic metaplasia states that cells that have a potential of becoming endometriosis are already present in the peritoneal lining of the pelvis. Those cells become activated due to environmental or hormonal factors then turn into endometriosis. Unfortunately, neither one of those theories fully explains all the cases of this disease which means that endometriosis may form in several different pathways (may be multifactorial).

Endometriosis implant on the abdominal wall. Bowel on the bottom.
Approximately 10% of women have endometriosis but only half will experience pelvic pain due to this condition. It may be present in about 70% of patients with pelvic pain, and about a third of patients who are undergoing laparoscopy for pain are found to have endometriosis. In patients who have laparoscopy for other reasons than pain 5% has endometriosis. Endometriosis may also lead to infertility which occurs in about 30% to 50% of patients with this condition. The rate of infertility in patients with endometriosis is 2 to 3 times higher than in general population.
Endometriosis is inheritable condition. Children and siblings of people with endometriosis are six times more likely to have this condition themselves. It is not known which genes are responsible for inheritance of endometriosis, but it appears that low level of progesterone hormone or progesterone receptor defect may increase the risk of this condition.
The most common symptom of endometriosis are painful menstrual periods. They occur in approximately two thirds of all the patients with this disease. Those painful periods usually start at the time of the first menstrual period (menarche) and with time get progressively worse. Eventually the pain is not only present during menstrual period but becomes continuous. Patients also experience pain with intercourse, urination, bowel movement and physical activity. Pain in endometriosis is mostly caused by uterine cramping but also cramping of the muscles of the pelvis and abdomen. Irritation of pelvic nerve endings and release of inflammatory substances is also responsible for the pain.
The only way to diagnose endometriosis is to perform surgery (laparoscopy or robotic laparoscopy) and visually confirme the presence of endometriosis implants. Because some conditions may resemble endometriosis, I strongly believe that pelvic lesions which look like endometriosis need to be removed and sent to pathology for microscopic confirmation.
Treatment of endometriosis may be medical or surgical. Medical treatment of endometriosis entails the use of medications which lower the levels of estrogens. Those medications may be effective, but they usually have side effects such as hot flashes, irritability, vaginal dryness and loss of libido. They generally mimic the symptoms that older patient would experience during menopause. Also, because of significant risk of osteoporosis, those medications should not be used for prolonged time. Unfortunately, when those medications are discontinued, endometriosis simply comes back. Research shows that medical treatment of endometriosis with anti-estrogen medications may be beneficial in mild form of endometriosis; in more severe cases they are not effective.
Surgical resection of endometriosis using robotic assisted laparoscopy or in some cases simple laparoscopy is the best treatment for this condition. Resection of endometriosis as opposed to ablation of endometriosis allows for much more precise removal of all the lesions minimizing the risk to vital pelvic and abdominal organs. This procedure, because of the complexity of pelvic anatomy, should be done by trained and experienced surgeon. Since endometriosis often involves bowels, bladder, diaphragm or other or abdominal/pelvic organ it is important that the surgeon is adequately trained to operate not only on reproductive organs but also on urinary and gastrointestinal systems. When lesions presumed to be endometriosis are resected, they should be then sent to the pathology to confirm that they are indeed endometriosis. There is ample research which shows that there are lesions appearing to be endometriosis which are not, and conversely endometriosis may sometimes appear like normal healthy tissue. Patients with severe endometriosis often develop endometriosis in the ovary. It is called an endometrioma. Endometriomas may cause significant pain but also are source of infertility. It is extremely important that surgery to remove endometrioma is done by a very experienced surgeon to preserve as much of a healthy ovary as possible for future fertility and hormone production.
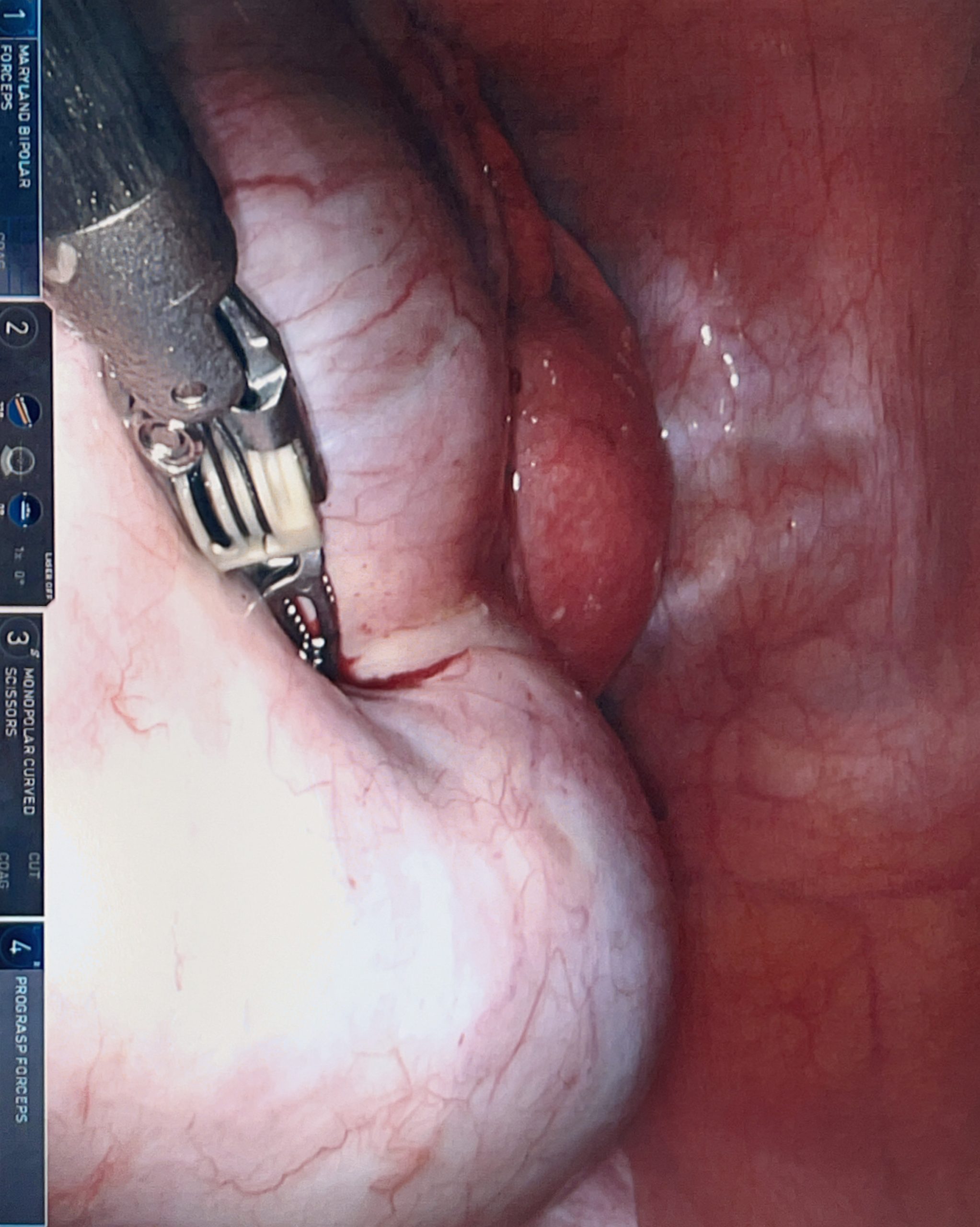
Ovarian endometrioma (bottom of the picture with da Vinci robot instrument pressing on it). Uterus on top of the picture
Surgical removal of endometriosis is successful in treatment of pelvic pain related to endometriosis. One of the most comprehensive studies demonstrated that patients who undergo surgical removal of endometriosis are 10 times less likely to have pain than those who just had diagnostic laparoscopy (surgery to look, without removing any endometriotic lesions). After surgical resection of endometriosis patients usually experience a long pain free period, but endometriosis will most likely return. Because we do not know how endometriosis happens in the first place, we do not know how to prevent it from re-occurring. In some cases (endometriosis in the ovary) birth control pills may delay the return of endometrioma, but in most of the cases birth control pills do not prevent or delay a relapse. A large study of over 850 women have shown that within five years from resection of endometriosis approximately half of the patients will have a reoccurrence of pain requiring another surgery.
In patients with endometriosis who are done with childbearing hysterectomy may be a good treatment option. Hysterectomy by itself does not prevent endometriosis from coming back, but because pain in patients with endometriosis is often from cramping of the uterus, it may prevent the reoccurrence of pain. In the study mentioned previously in seven years from the initial surgery 23% of patients who underwent hysterectomy had another surgery for endometriosis but only 8.3% of patients that had hysterectomy and ovaries removed needed another procedure.

Endometriosis on the diaphragm. Bottom of the picture – liver. Implants of endometriosis on the diaphragm fulgurated (coagulated) with argon beam coagulator.
Patient undergoing surgery for endometriosis may benefit from additional procedures in order to decrease pain. One of those procedures is presacral neurectomy. Presacral neurectomy is a procedure in which one of the nerves in the pelvis responsible for transmitting cramping sensation may be severed decreasing that sensation. Multiple studies have shown that patients with endometriosis undergoing presacral neurectomy have decreased pain (86% of patients are pain free one year from resection of endometriosis and presacral neurectomy versus 57% who just had resection of endometriosis). Presacral neurectomy is done in close proximity to very large pelvic veins (vena cava) and it should only be performed by very experienced surgeons.
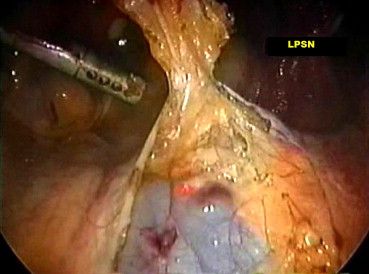
Presacral neurectomy with visible vena cava
One of the most important concepts in treatment of endometriosis is that it coexists with other pain causing conditions in the pelvis. For that reason, endometriosis has been called by some an “evil quadruplet”. The other three are spasm of the pelvic floor muscles, painful bladder syndrome (interstitial cystitis) and irritable bowel syndrome. When suffering from endometriosis it is very important to be treated by a physician who is not only trained and complicated resection of endometriosis but also can address those other conditions. Surgical resection of endometriosis without treatment of coexisting conditions may not bring the desired effects.
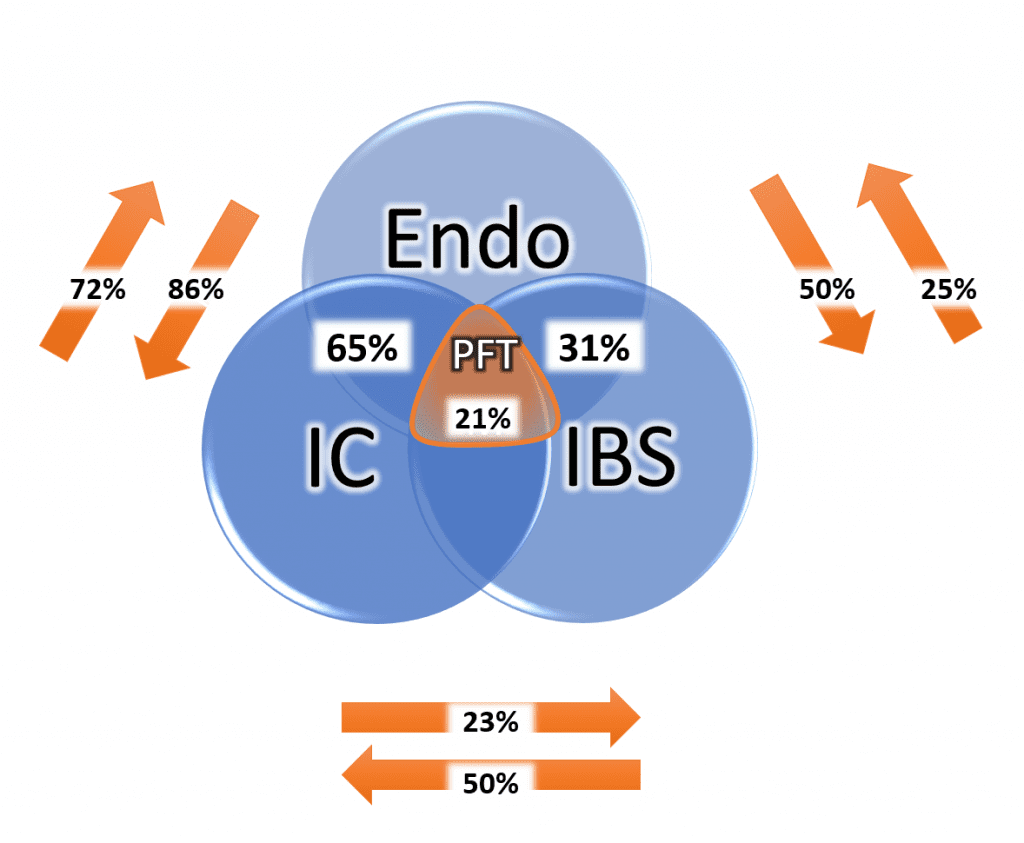
Conditions that coexist with endometriosis (IC – interstitial cystitis, IBS – irritable bowel syndrome, PFT – pelvic floor tension)
If you or anyone you know suffers from endometriosis, contact our office at 480 599-9682 or [email protected] to learn more about available treatments.
Robotic resection of mild endometriosis
Robotic resection of moderate endometriosis
Robotic resection of severe endometriosis and endometrioma
Robotic resection of diaphragm endometriosis
Presacral neurectomy
