Patient-Oriented Post Pudendal Nerve Decompression Surgery Handout
• Pudendal Nerve Decompression Surgery and Anatomy Education
The more you understand your body and interventions, the better your outcomes will be. You have been selected for this pudendal nerve procedure by Dr. Hibner with the utmost care based on your symptoms and progress or lack of with other disciplines and treatments. This is done to ensure you are the most appropriate candidate and will have the greatest chances of success with this surgery!
With pudendal nerve surgery, an incision is made into the buttock to expose the pudendal nerve. The point of the surgery is to remove scar tissue around the nerve and reduce pressure on the nerve, allowing you to have less pain or other symptoms. To achieve this, the sacrotuberous ligament is cut to allow Dr. Hibner access to the nerve ((c) below), which is reattached later in the pudendal nerve surgery.
This is part of why we do not want you to bend your hip at lot following surgery which is discussed later in this handout! We don’t want that ligament to come apart, it is part of what provides stability for this hip and pelvis.
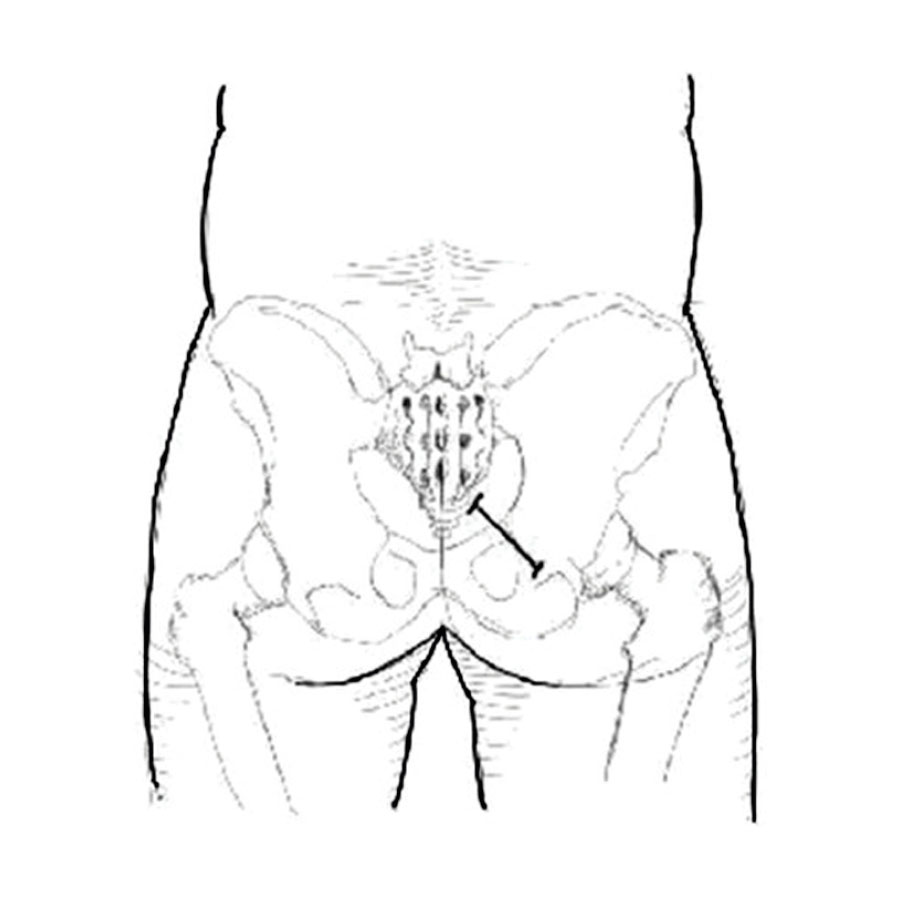
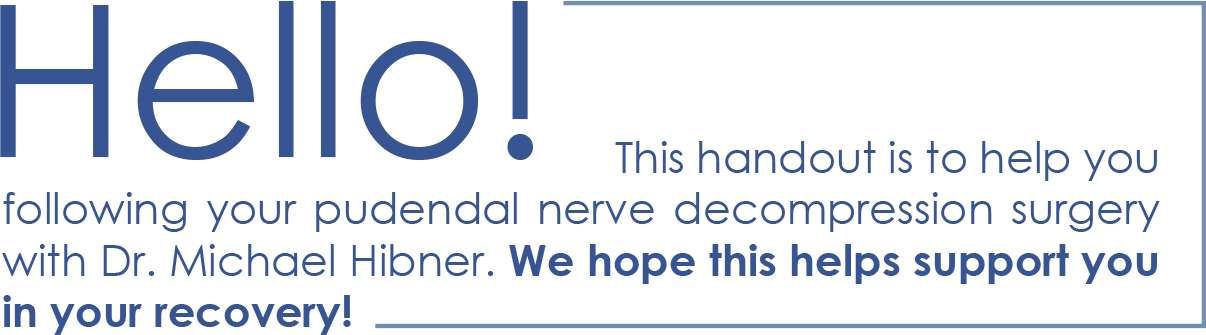
FIGURE 1: Location on the incision for transgluteal pudendal neurolysis
FIGURE 2: View through the right transgluteal incision. Skin, fat and gluteus muscle are incised.
(a) Pudendal neurovascular bundle.
(b) Sacrospinous ligament.
(c) Cut edges of sacrotuberous ligament.
(d) piriformis muscle. (e) Gluteus muscle
• What to Expect Following Pudendal Nerve Decompression Surgery
Immediately after surgery, you will have a urinary catheter. You will receive typical care following surgery meaning you will recover in a hospital room, will stay overnight, and will be discharged the next day. You will have an “On Q pain pump” which will release pain medication through a small catheter in your incision site. This will stay with you up to two weeks and you will be able to pull this out yourself at the end of that time. (We promise it is very easy).
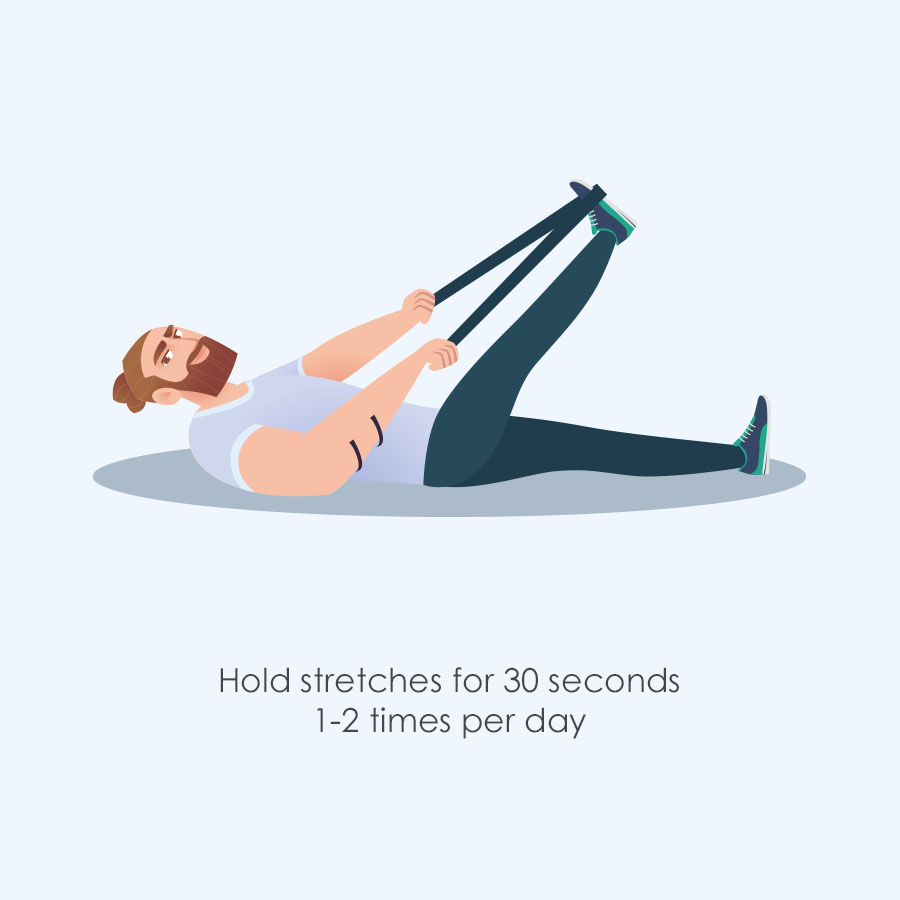
It is encouraged to walk after surgery the same day to reduce complications and improve outcomes. Morning after surgery it is encouraged to do “gliding” exercises of the hip. A couple examples of this are as follows. Try to do 5-10 repetitions at least once or more if tolerated on the operated leg if possible. Doing the other side won’t hurt either!
Remember these are only guidelines. Other general considerations following surgery: It is normal to experience increased symptoms at 6 months with maximum improvement noted at 18 months. Have you already scheduled your post op appointment with Dr. Hibner? This should be about 6 weeks after your surgery. How are you sleeping? Are you familiar with good sleep hygiene habits? How you sleep will affect your pain; if you are sleeping well you will have less pain! Are you working on your mind/body connection? Doing meditation, relaxation, yoga or other self care can help reduce your pain. Please contact Dr. Hibner’s office or your Physical Therapist if you have any questions or concerns.
• Other things to be aware of following surgery
Be aware of signs of infection such as: Fever, redness, fatigue, weakness, swelling, shaking or chills, heat or hardness to incision, and wound drainage. If any of these occur please contact Dr. Hibner’s office or another medical professional for appropriate direction.
• General Guidelines for Physical Activity following surgery
In general, we would like you to slowly increase your activity levels without placing too much strain on the surgery site as it heals. Everyone heals at a different rate and everyone has a different tolerance for pain. These guidelines are for all patients. It is important to listen to your body and do what is best for you. These guidelines only apply to the specific surgery by Dr. Michael Hibner.
0 - 3 Weeks After Surgery
Do and Don't
It will take 6-8 weeks for the surgery site to fully heal. Techniques to reduce your stress and improve relaxation are an important part of the recovery process. You can work on guided imagery, deep breathing, focused relaxation of muscles or any other techniques you find helpful.
Just concentrating on taking a deep breath into your belly will help. There are hundreds of resources online and in books that can be helpful. If you need more direction in this area, please talk to AZCCPP, your physical therapist, or other resources you have available to you.
Walking and exercise: We encourage you to walk as much as you can without causing any strong increase in pain. Often multiple short walks (4 or 5 1-10 min walks) are more comfortable than one long walk (1 walk of 20-30 mins). You don’t have to walk outside, walking around the house is fine. Avoid steep hills for the first few weeks. Continue completing hip gliding exercises twice a day.
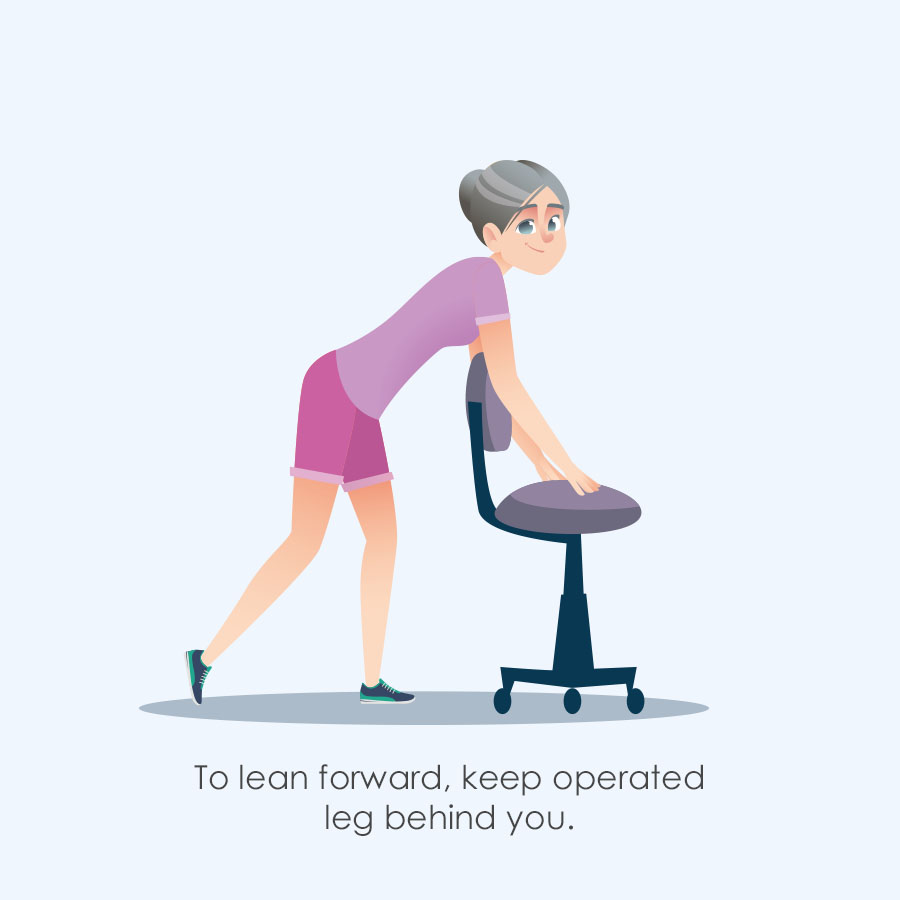
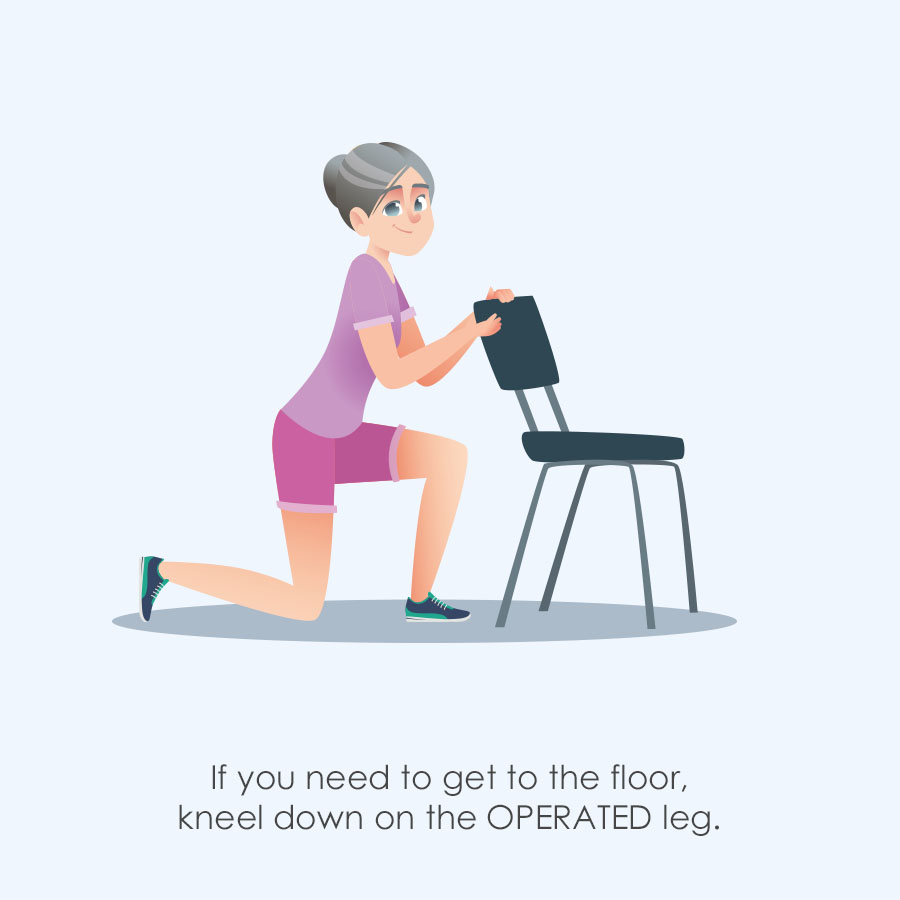
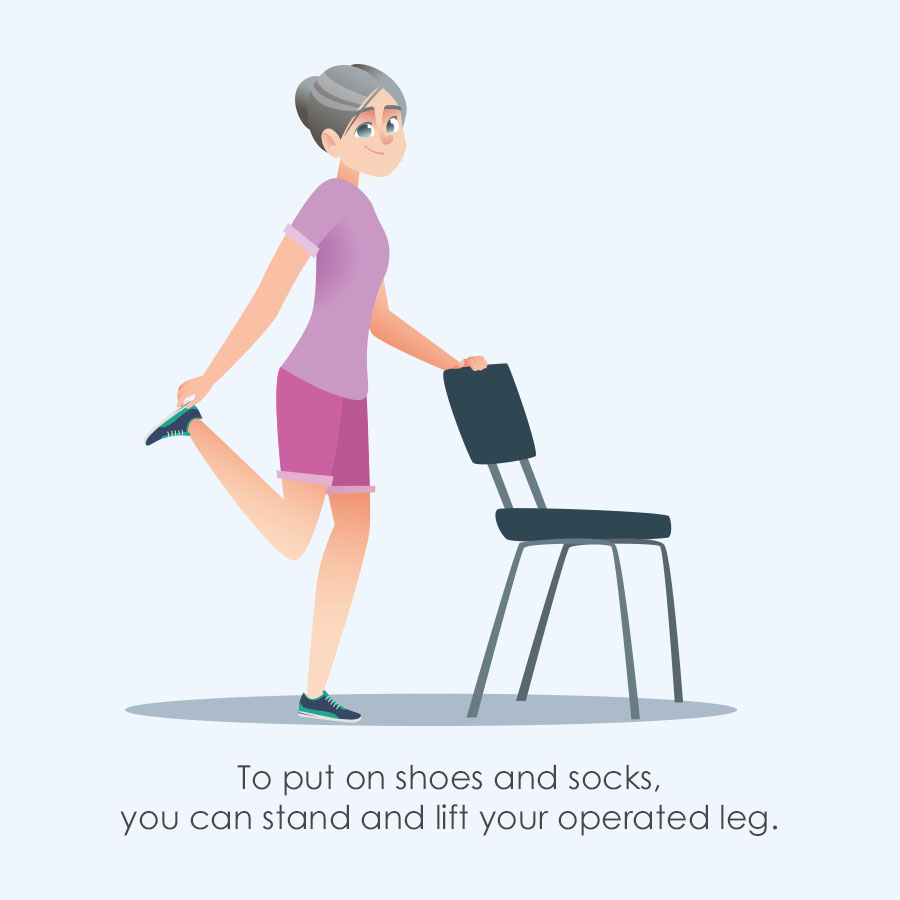
Dressing: Per precaution, do not pull knee to chest or bend fully forward. This means do not bend over to put on shoes or socks. Use slip on, or flip flops, or have someone else help you with your shoes. You can also lie on your back or side (see following for pictures). *You may want to use a sock puller or reacher. These can be obtained from a local drug store, medical supply store, or online. To put on underwear, shorts, or pants put operated leg in first. No full or deep squatting.
Sitting: You may want to avoid sitting or driving for the first 3-4 weeks. Most patients find it too uncomfortable to sit directly on the operated area for this first few weeks. It is okay to side sit, lie on either side, kneel, or lie on your back if that is more comfortable.
Stairs: Go up and down stairs one step at a time, not step over step. When going UP stairs, lead with UN-operated leg. When going DOWN stairs, lead with OPERATED leg. “Good” goes up, “bad” goes down.
Body Mechanics: The following pictures will help give you guidance about bending, squatting, and putting on shoes.
Post Pudendal Nerve Decompression Surgery:
The following examples will help you protect your surgery site. The examples are for an operation on the RIGHT leg.
Notice the hip does not bend more than 90 degrees tawards your chest. (90 degrees of HIP flexion)


3 - 8 Weeks Following Surgery
During this time frame progress is extremely variable between patients. Continue to listen to your body and do what is best for you.
Walking: Continue to increase walking as tolerated, avoiding steep hills. Walking is still the best exercise.
Exercise: Walking or gentle movements in the pool are fine if the incision is fully healed. NO hiking, bike riding, or strong stretching of the operated leg EVEN IF IT FEELS GREAT. It could potentially damage your surgery. (Remember the ligament that was reattached? THAT.) Your Physical Therapist can help provide more exercises as appropriate.
Sitting: You can slowly increase sitting on the surgery site. Continue using a cushion, it will be more comfortable. Try weight shifting initially. Meaning, sitting on the non-operated site, and then shifting to the operated side and putting 20% of your weight, then 40% of your weight, then 75% of your weight, etc. Work up to sitting more if tolerate. IF IT IS TOO PAINFUL TO SIT ON THE SURGERY AREA DO NOT DO IT. Everyone recovers at different rates. Listen to what is best for YOUR body.
Dressing: It is okay to gently start bending your hip a little bit more to get dressed.
Example Home Exercise Program (HEP) for less than 2 months after surgery:
Exercises examples beyond 2 months

8 Weeks and On
At this point your surgery site should be healed. You may still have significant pain, so please continue progressing at your own pace. Begin Physical Therapy if you have not already. Progress sitting as tolerated with using a cushion. Take stairs normally if comfortable, starting with smaller steps.

Remember these are only guidelines.
Other general considerations following surgery: It is normal to experience increased symptoms at 6 months with maximum improvement noted at 18 months. Have you already scheduled your post op appointment with Dr. Hibner? This should be about 6 weeks after your surgery. How are you sleeping? Are you familiar with good sleep hygiene habits? How you sleep will affect your pain; if you are sleeping well you will have less pain! Are you working on your mind/body connection? Doing meditation, relaxation, yoga or other self care can help reduce your pain.
Please contact Dr. Hibner’s office or your Physical Therapist if you have any questions or concerns.
