Embolotherapy, as a medical procedure, began gaining prominence in the United States in the late 1970s and early 1980s. Initially, it was introduced as a method for managing severe bleeding (hemorrhage) in emergency and surgical settings. Interventional radiology and catheter technology advancements were the driving forces behind its development.
The use of embolotherapy expanded significantly in the 1990s, with the introduction of more sophisticated embolic agents such as coils, particles, and liquid embolic. This progress allowed for targeted, minimally invasive treatment of various conditions, including uterine fibroids, liver tumors, and vascular malformations.
In the early 2000s, embolotherapy became a recognized treatment option for pelvic vein pressure and pelvic congestion syndrome (PCS). This came about after studies revealed that it successfully reduced pelvic varicose vein-related chronic pain. Since then, Pelvic Vein Embolization (PVE) has been increasingly adopted as a minimally invasive alternative to surgical procedures, offering high success rates with minimal recovery time.
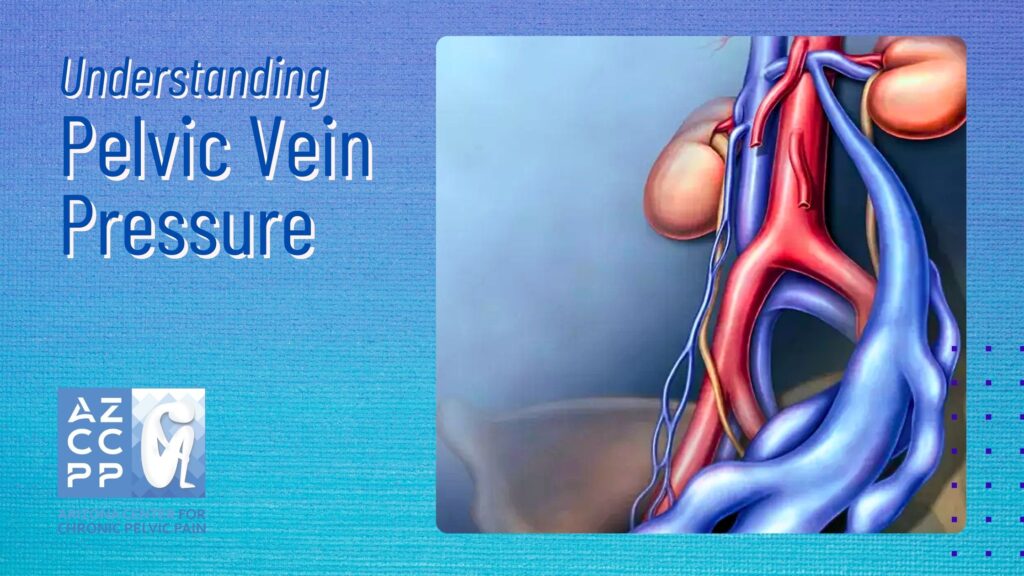
Understanding Pelvic Vein Pressure
This condition accounts for 10% of all gynecological office visits and 40% of laparoscopies annually. Given the significant impact of pelvic pain on individuals and healthcare systems, there is a pressing need for updated and detailed epidemiological studies to better understand and address this condition.
Pelvic vein pressure occurs when the veins in the pelvic region become abnormally dilated or varicose. This dilation results from increased pressure within the veins, often due to valve dysfunction that prevents proper blood flow. Instead of traveling efficiently back to the heart, blood pools in the pelvic veins, causing them to stretch, enlarge, and press on surrounding tissues and organs.
What Causes Pelvic Vein Pressure?
Pelvic vein pressure often develops due to the unique stressors placed on a woman’s body during certain life stages and activities, such as:
- Pregnancy: The growing uterus during pregnancy puts increased pressure on pelvic veins, and hormonal changes can weaken vein walls and valves, contributing to PCS.
- Hormonal Factors: High levels of estrogen can weaken vein walls, making women more susceptible to vein dilation.
- Multiple Pregnancies: Each pregnancy increases the likelihood of vein damage due to the repeated strain on the pelvic region.
- Prolonged Standing or Sitting: Occupations or habits that require extended periods of standing or sitting can worsen pelvic vein pressure by hindering blood flow.
- Genetics: A family history of varicose veins or other vascular conditions may increase the risk.
Common Symptoms of Pelvic Vein Pressure
Pelvic vein pressure manifests through various symptoms, often overlapping with other pelvic conditions. These symptoms can range from mild discomfort to severe pain that interferes with daily activities. Here are the key indicators:
- Chronic Pelvic Pain: This is the hallmark symptom of pelvic vein pressure. The pain is typically described as a dull, aching sensation that worsens.
- After standing for long periods due to increased blood pooling in the veins.
- Following sexual intercourse, is a phenomenon known as post-coital ache.
- During or after menstruation, hormonal fluctuations exacerbate the condition.
- Visible Varicose Veins: Varicose veins may appear in unusual locations, such as the buttocks, upper thighs, or vaginal area. These veins are often tender and may cause additional localized pain or discomfort.
- Menstrual Irregularities: Women with pelvic vein pressure often report heavier, longer, or more painful periods. These irregularities occur due to the increased blood volume and pressure in the pelvic region, which can affect the surrounding reproductive organs.
- Urinary Issues: The added pressure on the bladder and urinary tract can lead to symptoms such as:
- Increased urgency or frequency of urination.
- A sensation of incomplete bladder emptying.
- Pain or discomfort during urination.
Additional Symptoms to Watch For
While the above symptoms are the most common, some women may experience other signs of pelvic vein pressure, including:
- Lower Back Pain: Radiating pain that originates from the pelvic region and extends to the lower back.
- Pain During Physical Activity: Exercise, especially activities that increase abdominal pressure like running or heavy lifting, can worsen pelvic vein discomfort.
- Bloating and Heaviness: A persistent feeling of fullness or pressure in the lower abdomen, often described as a dragging sensation.
- Pain During Pregnancy: For women who develop pelvic vein pressure during pregnancy, symptoms can be more pronounced due to the additional vascular stress.
Impact on Quality of Life
Left untreated, pelvic vein pressure can severely affect a woman’s daily life. Chronic pain may lead to:
- Emotional and Psychological Strain: Persistent discomfort often causes anxiety, depression, and irritability.
- Interference with Intimacy: Pain during or after sexual intercourse may lead to strained relationships and decreased quality of life.
- Reduced Mobility: Women may avoid physical activities or standing for long periods due to exacerbated pain.
Understanding these symptoms and their underlying causes is crucial for early diagnosis and treatment. Seeking help from a pelvic pain treatment specialist or a chronic pain clinic in Arizona can provide the guidance and interventions needed to alleviate symptoms and improve overall health. Early intervention, including minimally invasive procedures like embolotherapy, offers a highly effective path to relief for women struggling with pelvic vein pressure.
Embolotherapy or Pelvic Vein Embolization (PVE): A Minimally Invasive Approach
Embolotherapy, also known as embolization, is a procedure that involves the intentional blockage of specific blood vessels to prevent blood flow to a targeted area. In the context of pelvic vein pressure, embolotherapy aims to block the problematic veins, reducing pressure and alleviating symptoms.
Procedure Overview:
- Access: A small catheter is inserted, typically through the groin or neck.
- Navigation: Using imaging guidance, the catheter is directed to the affected pelvic veins.
- Embolic Agents: Materials such as coils or sclerosing agents are introduced to occlude the veins.
- Completion: The catheter is removed, and the entry point is bandaged.
Advantages of Embolotherapy:
- Minimally Invasive: No large incisions, leading to reduced recovery time.
- High Success Rates: Many patients experience significant symptom relief.
- Outpatient Procedure: Often performed without the need for hospital admission.
Pelvic Pain Treatment in Arizona
Arizona boasts a range of specialized clinics and practitioners dedicated to treating pelvic pain. One notable institution is the Arizona Center for Chronic Pelvic Pain (AZCCPP), led by Dr. Michael Hibner, a renowned Female Pelvic Medicine & Reconstructive Surgeon.
Comprehensive Care at AZCCPP:
- Multidisciplinary Approach: Combining gynecology, urology, and pain management.
- Personalized Treatment Plans: Tailored to each patient’s unique condition.
- Advanced Diagnostic Tools: Ensuring accurate identification of underlying causes.
“Embolotherapy has revolutionized the way we approach pelvic vein pressure. By targeting the source of the problem, we can offer patients relief without the need for invasive surgery.” – Dr. Michael Hibner
Dr. HIbner adds, “At AZCCPP, our goal is to provide holistic care. We understand that chronic pelvic pain affects every aspect of a woman’s life, and we’re committed to restoring health and well-being.”
Conclusion
Embolotherapy stands as a beacon of hope for women grappling with pelvic vein pressure. Its minimally invasive nature, coupled with high success rates, makes it a compelling option for those seeking relief. In Arizona, clinics like AZCCPP, under the expert guidance of Dr. Michael Hibner, are at the forefront of providing specialized pelvic pain treatment, ensuring that patients receive comprehensive and compassionate care.
Take the Next Step Towards Relief
If you’re experiencing symptoms of pelvic vein pressure, don’t wait to seek help. At the Arizona Center for Chronic Pelvic Pain (AZCCPP), we specialize in diagnosing and treating pelvic floor disorders. Our team, led by Dr. Michael Hibner, is dedicated to providing personalized care tailored to your needs.
Why Choose AZCCPP?
- Expertise: Dr. Hibner brings extensive experience in pelvic medicine and reconstructive surgery.
- Comprehensive Care: We offer a multidisciplinary approach, ensuring all aspects of your condition are addressed.
- Patient-Centered Approach: Your comfort and well-being are our top priorities.
READ MORE: Pelvic Congestion Syndrome in Women
Pelvic Congestion Syndrome in Women: 10 Common Questions Answered
Contact Us for Pelvic Vein Pressure Treatment for Women
Take control of your health and find relief from Pelvic Vein Pressure. Connect with us to discuss your symptoms, get answers to your questions, and receive expert guidance for managing this condition. Book a personalized consultation by calling (480) 599-9682 or emailing [email protected]. Let’s work together to bring you comfort, clarity, and a renewed sense of well-being. Visit the Arizona Center for Chronic Pelvic Pain to explore our services and see how we can support your journey.
Check out AZCCPP on YouTube for more questions that need answers with Dr. Michael Hibner.

