Prostatitis, an inflammation of the prostate gland, presents a unique challenge in the diagnosis and management of prostate-related conditions. In men with prostatitis, the need for accurate diagnosis becomes paramount, especially when symptoms overlap with other prostate conditions, such as prostate cancer. One of the most definitive diagnostic tools available is the prostate biopsy. This article delves into the intricate relationship between prostatitis and prostate biopsy, providing a comprehensive guide for men facing this procedure.
Prostatitis: A Complex Condition
Prostatitis encompasses a range of conditions that cause inflammation of the prostate gland. These include acute bacterial prostatitis, chronic bacterial prostatitis, chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), and asymptomatic inflammatory prostatitis. The symptoms of prostatitis can vary widely but often include pelvic pain, urinary difficulties, and sexual dysfunction. The presence of inflammation can complicate the clinical picture, making it challenging to distinguish prostatitis from other conditions such as benign prostatic hyperplasia (BPH) and prostate cancer.
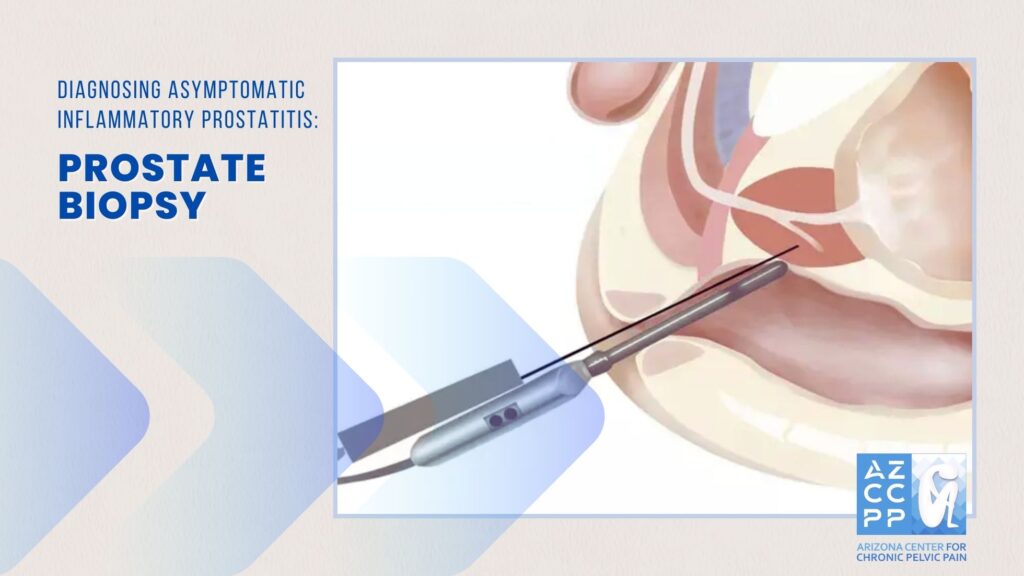
Diagnosing AIP: Why Prostate Biopsy May Be Necessary
In men with prostatitis, determining the underlying cause of symptoms is crucial. When elevated prostate-specific antigen (PSA) levels are detected, or when a digital rectal examination (DRE) reveals abnormalities, the suspicion of prostate cancer may arise. However, prostatitis itself can cause elevated PSA levels, leading to diagnostic uncertainty. A prostate biopsy becomes essential in these cases to differentiate between prostatitis and prostate cancer, enabling appropriate treatment decisions.
Types of Prostate Biopsy
Several biopsy techniques are available, each with specific indications and advantages:
1. Transrectal Ultrasound-Guided Biopsy (TRUS)
- TRUS biopsy is the most common method used. It involves the insertion of an ultrasound probe into the rectum to guide the biopsy needle to the prostate. Multiple tissue samples are taken from different areas of the prostate to ensure comprehensive evaluation.
2. Transperineal Biopsy
- In this method, the biopsy needle is inserted through the perineum (the area between the scrotum and the anus) rather than the rectum. This approach reduces the risk of infection, which is particularly important in patients with chronic prostatitis.
3. MRI/Ultrasound Fusion-Guided Biopsy
- This advanced technique combines the anatomical detail of MRI with the real-time guidance of ultrasound. It is especially useful for targeting suspicious areas identified on MRI, potentially improving the accuracy of cancer detection in men with prostatitis.
Preparation for Prostate Biopsy
Preparation for a prostate biopsy involves several key steps to minimize complications and ensure accurate results:
- Antibiotic Prophylaxis: Given the increased risk of infection associated with prostatitis, antibiotics are typically administered before and after the biopsy. This is crucial in reducing the risk of sepsis, a severe systemic infection.
- Bowel Preparation: Patients may be advised to undergo bowel preparation to reduce the bacterial load in the rectum, particularly for TRUS biopsy.
- PSA Levels: The timing of PSA testing in relation to a biopsy is important. PSA levels may be temporarily elevated following a biopsy or prostatitis flare-up, so careful consideration is needed when interpreting results.
The Procedure: What to Expect
During the biopsy, patients can expect the following:
- Anesthesia: Local anesthesia is typically used to numb the area and reduce discomfort. In some cases, sedation may be provided.
- Positioning: The patient is positioned on their side or back, depending on the biopsy method.
- Biopsy Sampling: The biopsy needle is inserted, and multiple samples are taken. The entire procedure usually takes about 10 to 15 minutes.
- Post-Biopsy Care: After the procedure, patients are monitored for a short period to ensure there are no immediate complications.
Interpreting Biopsy Results
The tissue samples obtained during the biopsy are analyzed by a pathologist to determine the presence of cancerous cells. In men with prostatitis, the pathologist will also assess the degree of inflammation and look for other potential causes of elevated PSA levels.
- Negative Biopsy: A negative result indicates no evidence of cancer. However, if prostatitis is present, ongoing management of inflammation is necessary.
- Positive Biopsy: A positive result confirms the presence of prostate cancer, and further staging and treatment planning will be required.
Risks and Complications of Prostate Biopsy
While prostate biopsy is generally safe, certain risks and complications are more pronounced in men with prostatitis:
- Infection: The risk of infection is heightened in patients with prostatitis due to the pre-existing inflammation and potential bacterial presence. Symptoms of infection, such as fever, chills, and urinary difficulties, should be promptly addressed.
- Bleeding: Hematuria (blood in the urine) and rectal bleeding are common post-biopsy but usually resolve within a few days. Persistent bleeding should be evaluated by a healthcare provider.
- Urinary Retention: In some cases, swelling or inflammation following the biopsy can lead to temporary urinary retention. This requires immediate medical attention.
- Pain and Discomfort: While mild discomfort is expected, significant pain should be reported to a healthcare provider, as it may indicate an underlying complication.
Post-Biopsy Follow-Up
Follow-up care after a prostate biopsy is crucial, especially for men with prostatitis. The following steps are typically recommended:
- Monitoring PSA Levels: PSA levels should be re-evaluated several weeks after the biopsy to assess any changes related to the procedure or underlying conditions.
- Managing Prostatitis: Ongoing treatment for prostatitis, such as antibiotics, anti-inflammatory medications, or lifestyle modifications, may be necessary to control symptoms and prevent flare-ups.
- Further Testing: In cases where the biopsy results are inconclusive or where prostatitis obscures the diagnosis, additional imaging studies or repeat biopsies may be required.
Conclusion
For men with prostatitis, the decision to undergo a prostate biopsy is complex and requires careful consideration of the potential benefits and risks. While prostatitis can complicate the diagnostic process, a biopsy remains a crucial tool in distinguishing between benign inflammatory conditions and prostate cancer. Through accurate diagnosis and appropriate management, men can achieve better outcomes and reduce the impact of prostate-related conditions on their quality of life.
READ MORE: On Men’s Health: What Is Asymptomatic Inflammatory Prostatitis
On Men’s Health: What Is Asymptomatic Inflammatory Prostatitis
Contact Us for Chronic Pelvic Pain Treatment for Men
If you’re experiencing symptoms of Asymptomatic Inflammatory Prostatitis or AIP, don’t delay seeking medical attention. Contact the Arizona Center for Chronic Pelvic Pain for expert diagnosis and personalized treatment. Our experienced team specializes in managing pelvic pain conditions and can provide the care you need to feel better. Call us at (480) 599-9682 or email [email protected] to schedule an appointment.
AZCCPP offers comprehensive evaluation, personalized treatment plans, and compassionate care to help you find relief. Contact us today at (480) 599-9682 or [email protected] to schedule an appointment. You may also check out AZCCPP on YouTube for more questions that need answers with Dr. Michael Hibner.
By understanding the symptoms, causes, diagnosis, and treatment options for Asymptomatic Inflammatory Prostatitis, you can take proactive steps to manage this condition effectively and regain your quality of life.