Discover the hidden aspects of asymptomatic inflammatory prostatitis—how it’s detected, its potential health implications, and why monitoring prostate health is crucial, even in the absence of symptoms.
Asymptomatic Inflammatory Prostatitis or AIP: Understanding a Silent Condition
Asymptomatic inflammatory prostatitis is a condition characterized by inflammation of the prostate gland without the presence of any accompanying symptoms. Although it may not manifest with noticeable signs, it is a significant clinical condition that can have implications for long-term prostate health.
It is often detected incidentally during routine medical evaluations or screening tests, such as those performed for prostate cancer. Despite its silent nature, asymptomatic inflammatory prostatitis requires careful consideration due to its potential impact on the prostate and overall male health.
What is Asymptomatic Inflammatory Prostatitis?
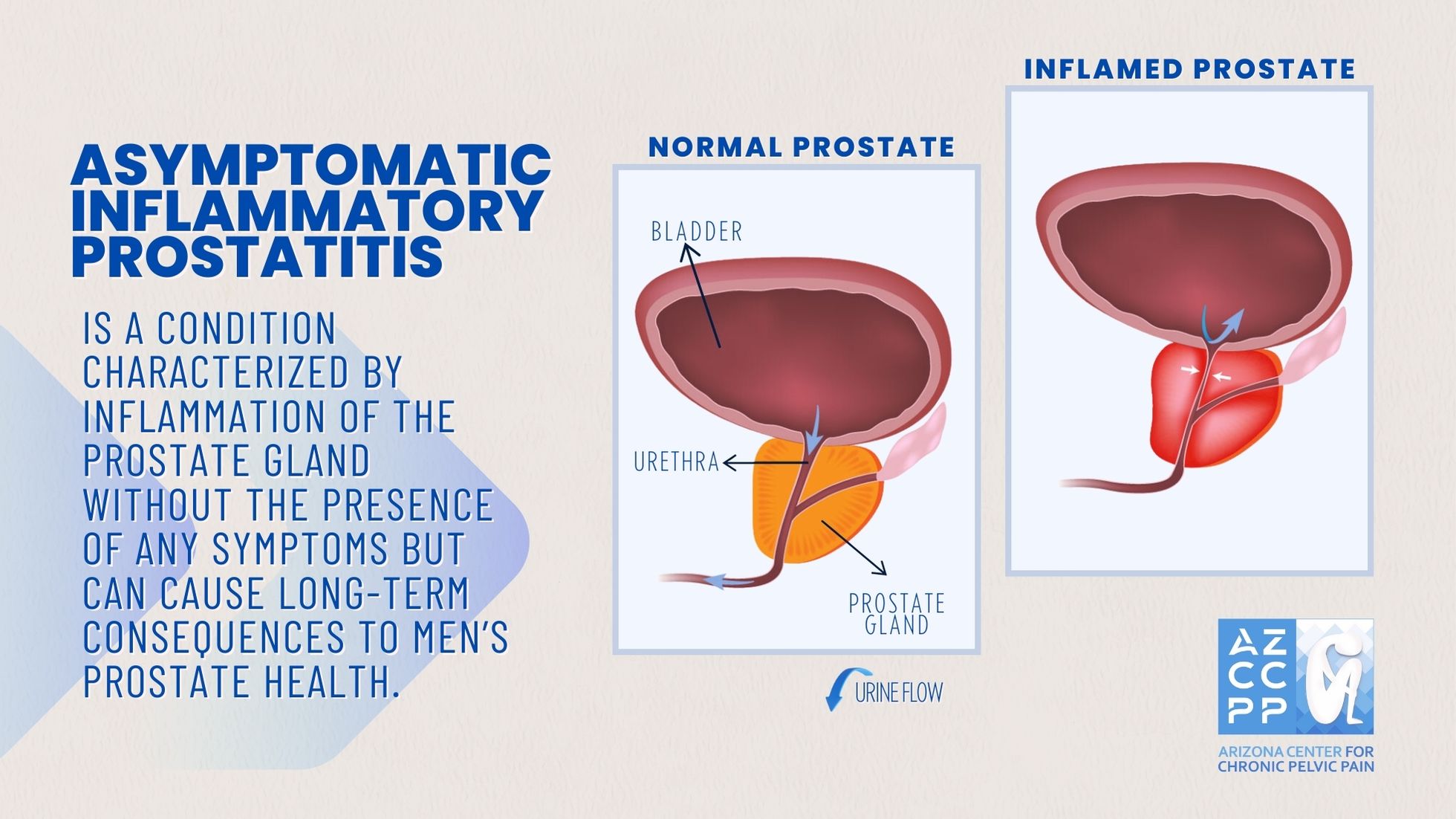
The prostate gland is a small, walnut-shaped gland located just below the bladder and in front of the rectum in males. It plays a crucial role in male reproductive function by producing seminal fluid, which is a component of semen. The health of the prostate is vital for both urinary and reproductive functions.
Inflammation of the prostate gland, known as prostatitis, can occur with or without symptoms, and it is categorized into four types according to the National Institutes of Health (NIH) classification system: acute bacterial prostatitis, chronic bacterial prostatitis, chronic pelvic pain syndrome (CPPS), and asymptomatic inflammatory prostatitis.
Asymptomatic inflammatory prostatitis falls under Category IV of the NIH classification. This condition is characterized by the presence of white blood cells in the prostate gland or seminal fluid without the presence of symptoms typically associated with prostatitis, such as pelvic pain, urinary symptoms, or sexual dysfunction.
This absence of symptoms makes it distinct from other forms of prostatitis, which are often associated with significant discomfort and quality-of-life impairments.
Epidemiology and Prevalence
Asymptomatic inflammatory prostatitis is more common than previously thought, often being detected during evaluations for other prostate conditions, such as benign prostatic hyperplasia (BPH) or prostate cancer. Studies suggest that it may be present in up to 40–50% of men who undergo a biopsy or prostatectomy for reasons unrelated to prostatitis.
The condition’s prevalence increases with age, which aligns with the general increase in prostate-related issues in older men. However, it can also be found in younger men who are being evaluated for infertility or other reproductive concerns.
Pathophysiology and Etiology
The exact cause of asymptomatic inflammatory prostatitis is not well understood, but it is believed to be multifactorial. Theories regarding its etiology include:
- Infectious Agents: Although bacteria are not typically cultured from patients with asymptomatic inflammatory prostatitis, some studies suggest that subclinical infections or non-bacterial pathogens might play a role in initiating or sustaining inflammation.
- Autoimmune Mechanisms: Autoimmune responses may contribute to the inflammation seen in this condition. The presence of white blood cells in the prostate without a clear infectious cause suggests that an autoimmune process might be involved, where the body’s immune system mistakenly targets prostate tissue.
- Chemical Irritation: Reflux of urine into the prostate ducts, known as intraprostatic reflux, can lead to chemical irritation and subsequent inflammation. This process might occur silently, without causing symptoms in the patient.
- Hormonal Imbalances: Hormonal changes, particularly those involving testosterone and dihydrotestosterone (DHT), may contribute to the development of prostate inflammation, even in the absence of symptoms.
- Genetic Predisposition: Some men may have a genetic predisposition to develop inflammation in the prostate gland, which could explain why asymptomatic inflammatory prostatitis is found in some individuals and not others.
Diagnosis of Asymptomatic Inflammatory Prostatitis
Diagnosing asymptomatic inflammatory prostatitis is often challenging due to the lack of symptoms. The condition is usually discovered incidentally during routine prostate evaluations, which may include:
1. Prostate-Specific Antigen (PSA) Testing
PSA is a protein that both healthy and inflamed prostate tissue produce. Elevated PSA levels are commonly associated with prostate cancer, but they can also be elevated in cases of prostatitis, including asymptomatic inflammatory prostatitis. An unexplained rise in PSA levels during routine screening might prompt further investigation. Prostate-specific antigen (PSA) testing in men with prostatitis requires careful interpretation to avoid a misdiagnosis. By following clinical guidelines and considering individual patient factors, we can improve the accuracy of diagnosis and patient outcomes in this challenging scenario.
PSA testing is a critical tool in diagnosing prostate conditions, but its interpretation becomes complex in men with prostatitis. Prostatitis, an inflammation of the prostate, can cause elevated PSA levels, which are typically associated with prostate cancer. This overlap often leads to diagnostic challenges.
Prostatitis can manifest as acute bacterial prostatitis, chronic bacterial prostatitis, chronic pelvic pain syndrome (CPPS), or asymptomatic inflammatory prostatitis. Each form can result in PSA elevation, complicating the differentiation from prostate cancer. To accurately interpret PSA levels in this context, clinicians should consider serial PSA measurements, PSA density, and the free-to-total PSA ratio. These methods can help distinguish between PSA elevations due to inflammation and those suggestive of malignancy.
PSA testing should not be conducted during an acute episode of prostatitis, as this can yield falsely elevated results. It’s advisable to wait several weeks post-treatment before retesting. Persistent PSA elevation after prostatitis treatment may warrant further investigation, including a potential biopsy, though this decision should be made cautiously to avoid unnecessary procedures.
For men with chronic prostatitis, ongoing PSA monitoring is often necessary. Lifestyle modifications, such as dietary adjustments and stress management, may help stabilize PSA levels and manage symptoms.
2. Digital Rectal Examination (DRE)
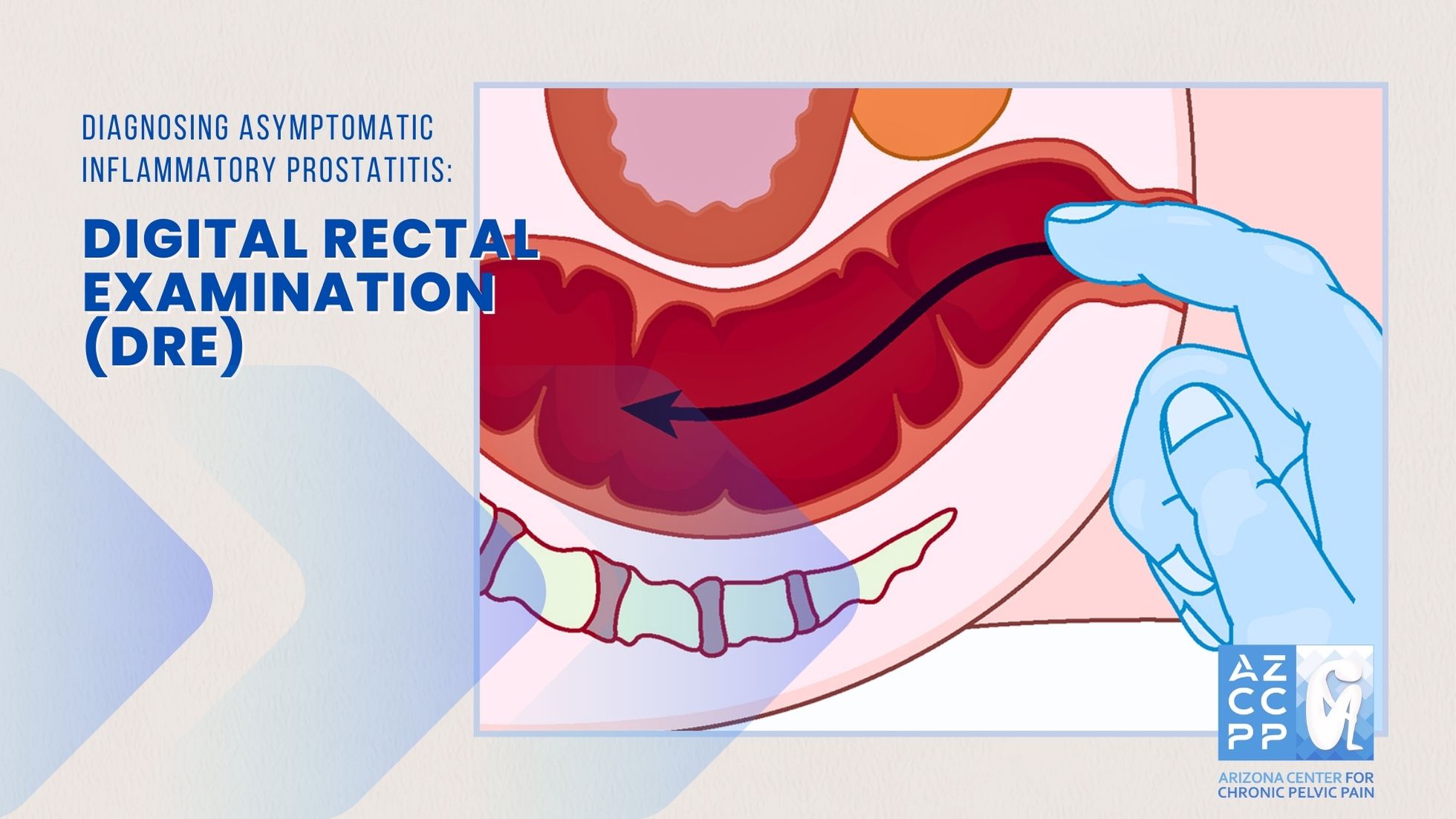
A DRE is a quick and essential test for detecting prostate issues early, leading to better health outcomes. It helps doctors evaluate the health of the lower rectum and prostate gland. During the exam, a healthcare provider inserts a lubricated, gloved finger into the rectum to check for prostate cancer, tumors, or other abnormalities. A DRE may be recommended for men experiencing:
- Blood in the stool
- Rectal bleeding
- Changes in bowel habits
- Unusual discharge from the urethra
- Changes in urine flow
- Routine screening for prostate cancer
- Diagnosis of rectal tumors
- Assessment of hemorrhoids
Before the exam, inform your doctor if you have any existing conditions in the anal area, such as hemorrhoids or anal fissures. This information helps the doctor perform the exam with minimal discomfort.
The DRE is straightforward:
- Positioning: You may be asked to stand and bend forward or lie on your side with knees drawn up.
- Relaxation: Your doctor will ask you to relax and take a deep breath.
- Examination: A lubricated, gloved finger is gently inserted into the rectum. The doctor checks the anal tone by asking you to squeeze around the finger and examines the prostate gland for any lumps or irregularities.
- Completion: The exam takes only a few minutes. The finger is removed, and the glove is checked for any signs of blood or abnormal tissue.
You can resume normal activities right after the exam. Some men may experience slight discomfort or minor rectal bleeding if they have hemorrhoids, but these symptoms usually resolve quickly. If the doctor detects any abnormalities, further testing may be recommended.
3. Prostate Biopsy
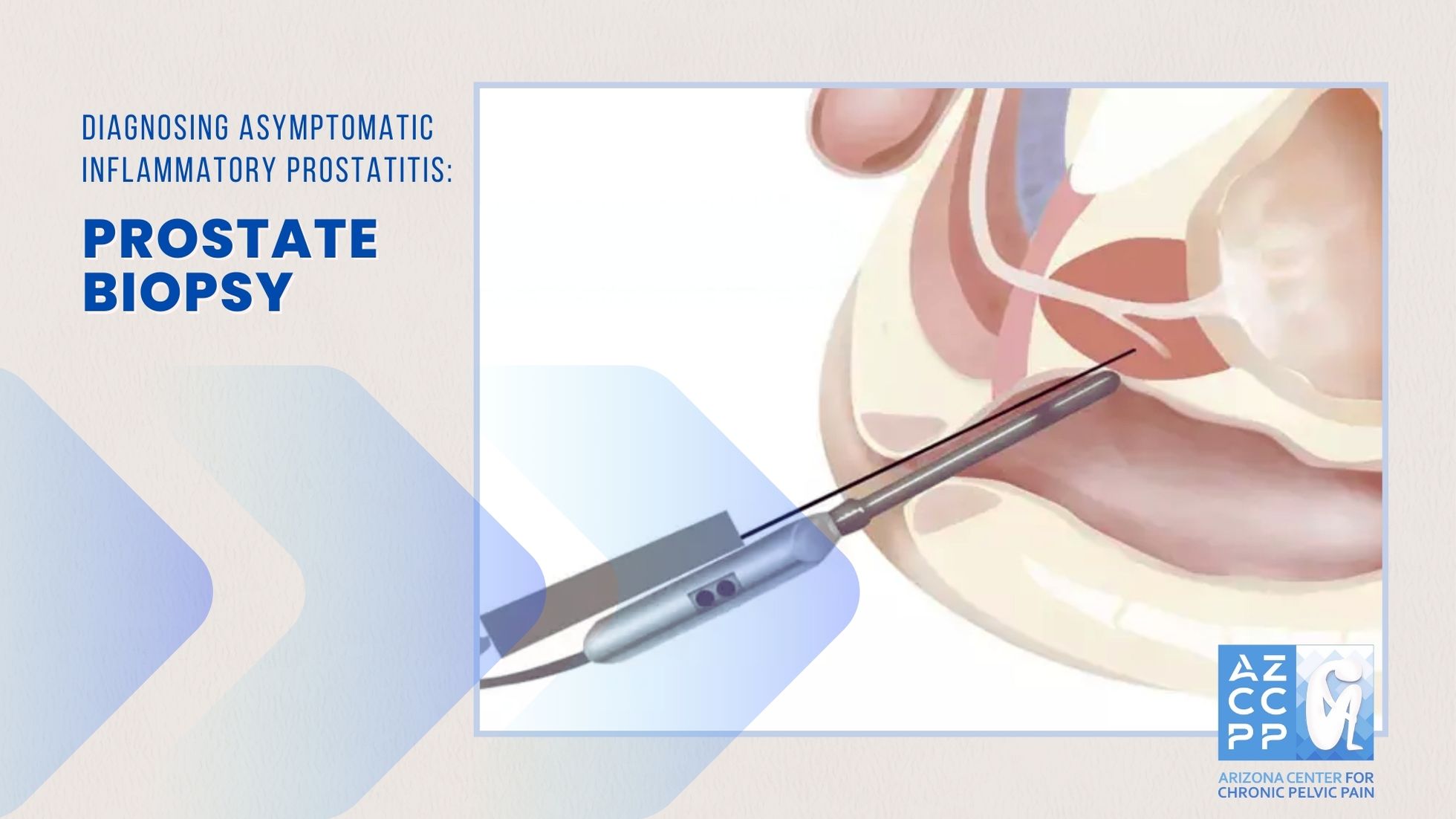
Prostatitis, the inflammation of the prostate gland, often presents with symptoms that overlap with other prostate conditions, such as prostate cancer. This overlap can complicate diagnosis, making a prostate biopsy a crucial tool when elevated PSA levels or abnormalities in a digital rectal examination (DRE) are detected.
A prostate biopsy involves extracting small tissue samples from the prostate to determine the presence of cancer. In men with prostatitis, this procedure is essential to distinguish between inflammation and malignancy. There are several biopsy techniques available, including the commonly used Transrectal Ultrasound-Guided Biopsy (TRUS), the Transperineal Biopsy, which minimizes infection risks, and the MRI/Ultrasound Fusion-Guided Biopsy for targeting suspicious areas.
Preparation for the biopsy includes antibiotic prophylaxis to reduce infection risks, especially important in those with prostatitis. The procedure itself is brief, usually taking 10-15 minutes, and involves local anesthesia. Post-biopsy care focuses on monitoring for complications such as infection, bleeding, and urinary retention.
Interpreting biopsy results is critical. A negative result may still require ongoing management of prostatitis, while a positive result will lead to further cancer treatment planning. Although the biopsy is generally safe, men with prostatitis must be vigilant about potential complications and follow up with their healthcare provider for continued management of their condition.
4. Semen Analysis

Asymptomatic Inflammatory Prostatitis (AIP) is a condition that causes inflammation of the prostate without obvious symptoms. Semen analysis is crucial for detecting AIP, as it reveals leukocytes and inflammatory markers in the semen.
Key diagnostic indicators include:
- Leukocytospermia: Elevated white blood cells in semen suggest prostatic inflammation.
- Inflammatory Markers: Increased levels of pro-inflammatory cytokines like IL-6, IL-8, and TNF-α indicate inflammation.
- Microbiological Examination: Detects pathogens in semen, guiding appropriate treatment if a bacterial cause is identified.
Semen analysis helps in early detection of AIP, which is vital for preventing complications and managing fertility issues. Inflammatory changes can impact sperm quality, leading to reduced fertility, so identifying and treating AIP can enhance reproductive outcomes. Additionally, it aids in determining targeted treatments, whether antibiotic or anti-inflammatory, tailored to the patient’s specific condition.
As such, semen analysis is an effective diagnostic tool for AIP, offering insights into prostatic health and its effects on fertility. Early identification and treatment are essential for improving patient outcomes and managing associated fertility problems.
Clinical Significance and Implications
While asymptomatic inflammatory prostatitis does not cause discomfort, its presence can have significant clinical implications. For instance, chronic inflammation of the prostate has been hypothesized to play a role in the development of more serious conditions, such as prostate cancer.
Several studies have explored the potential link between chronic inflammation and carcinogenesis in the prostate, suggesting that long-standing inflammation may create an environment conducive to cancer development.
Furthermore, asymptomatic inflammatory prostatitis may complicate the interpretation of PSA test results, leading to unnecessary biopsies or overtreatment. Elevated PSA levels in the absence of prostate cancer can result from inflammation, and distinguishing between benign causes of PSA elevation and malignancy is crucial for appropriate patient management.
Treatment Considerations
The management of asymptomatic inflammatory prostatitis is controversial due to its lack of symptoms. In many cases, no treatment is necessary, and a watchful waiting approach may be adopted. However, in certain scenarios, healthcare providers may consider interventions based on individual factors:
- Observation: For many men, especially those without symptoms or complications, regular monitoring of prostate health may be sufficient. This approach avoids the risks associated with unnecessary treatments and focuses on maintaining quality of life.
- Medications: In cases where there is concern about potential complications or when inflammation is detected in the context of other prostate conditions, healthcare providers may prescribe anti-inflammatory medications or antibiotics. The use of antibiotics is particularly controversial in the absence of bacterial infection, and their use should be carefully considered.
- Lifestyle Modifications: Some studies suggest that lifestyle changes, such as diet modifications, exercise, and stress management, may help reduce inflammation and support prostate health. While evidence is limited, these interventions are generally low-risk and may have additional health benefits.
Conclusion
Asymptomatic inflammatory prostatitis is a complex and often overlooked condition that requires a nuanced understanding. Although it does not cause noticeable symptoms, its potential implications for prostate health, particularly in relation to PSA testing and the risk of prostate cancer, make it a condition worth monitoring. Men diagnosed with asymptomatic inflammatory prostatitis should engage in regular follow-ups with their healthcare providers to ensure that their prostate health is maintained and to address any emerging concerns proactively.
For those seeking expert guidance on prostate health, including conditions like asymptomatic inflammatory prostatitis, the Arizona Center for Chronic Pelvic Pain offers specialized care. Their experienced team provides comprehensive evaluation and personalized treatment plans to help maintain prostate health and overall well-being. Contact the Arizona Center for Chronic Pelvic Pain at (480) 599-9682 or [email protected] to schedule a consultation.
READ MORE: On Men’s Health: Understanding Acute Bacterial Prostatitis
Contact Us for Chronic Pelvic Pain Treatment for Men
If you’re experiencing symptoms of Asymptomatic Inflammatory Prostatitis, don’t delay seeking medical attention. Contact the Arizona Center for Chronic Pelvic Pain for expert diagnosis and personalized treatment. Our experienced team specializes in managing pelvic pain conditions and can provide the care you need to feel better. Call us at (480) 599-9682 or email [email protected] to schedule an appointment.
AZCCPP offers comprehensive evaluation, personalized treatment plans, and compassionate care to help you find relief. Contact us today at (480) 599-9682 or [email protected] to schedule an appointment. You may also check out AZCCPP on YouTube for more questions that need answers with Dr. Michael Hibner.
By understanding the symptoms, causes, diagnosis, and treatment options for Asymptomatic Inflammatory Prostatitis, you can take proactive steps to manage this condition effectively and regain your quality of life.